- What is Male Breast Cancer (Male Breast Carcinoma)?
- Statistics
- Risk Factors
- Progression
- Symptoms
- Clinical Examination
- How is it Diagnosed
- Prognosis
- Treatment
- References
What is Male Breast Cancer (Male Breast Carcinoma)?
Male breast cancer is a rare but important disease. Many people do not realise that men, as well as women, have breast tissue. In women, the breast is composed mainly of fatty tissue, milk glands and a series of ducts connecting the glands to the nipple. In men, only a small amount of breast tissue is present. This is mainly made up of fat, with a few ducts and some connective tissue. However, this small amount of breast tissue can occasionally undergo malignant (cancerous) change, producing breast cancer. Breast cancer in men is essentially the same disease as breast cancer in women. A few important differences do exist, and these are discussed below.
Statistics
Breast cancer in men is rare; of the 14,568 breast cancers in Australia in 2011, just 103, or less than 1%, were diagnosed in males. 1 per 100,000 men are diagnosed with breast cancer each year, compared to 125 per 100,000 for females and breast cancer in men is not increasing.
A man’s risk of developing breast cancer increases with age and in 719 men will be diagnosed with breast cancer before their 85th birthday. On average men are 69 years of age when first diagnosed with breast cancer, compared to 60 years old for women. The majority (85%) of breast cancer in men are invasive ductal carcinoma (arising in the ductal tissues of the breast.
Male breast cancer is more common in some countries including Egypt (6% of all breast cancers) and Zambia (15% of all breast cancers). This is thought to relate to the increased incidence of liver disease which causes men to produce more oestrogen, a hormone which plays a role in the development of breast cancer. Incidence is lower in Japan and higher in North America and Great Britain.
Risk Factors
Predisposing factors for male breast cancer include:
- Radiation exposure: previous radiation treatment to the chest, for example for Hodgkin’s lymphoma, increases the risk of developing breast cancer.
- Increased oestrogen: oestrogen is a female sex hormone that triggers the growth of breast tissue. Males can have increased exposure to oestrogen through some drugs (used in the treatment of prostate cancer). Diseases affecting the liver (such as cirrhosis) can inhibit oestrogen clearance from the body. A disorder known as Klinefelter’s syndrome, where males have an extra X chromosome, is also associated with elevated levels of oestrogen.
- Obesity: this increases the number of fat cells in the body which convert androgens (male sex hormones) into oestrogen.
- Family history: breast cancer is up to 2.5 times more common in men with first degree female relatives with breast cancer.
- Genetics: Male breast cancer is strongly associated with a gene mutation known as BRCA2. Men with this mutation are approximately one hundred times more likely to get breast cancer than those without. Genetic tests can determine whether this mutation is present. There is no increased risk to men with the BRCA1 mutation.
- Increasing age: as mentioned, the majority of breast cancers are diagnosed between the ages of 60 and 70.
- Testicular abnormalities: some conditions involving abnormalities of the testes, including orchitis (testicular infection), undescended testes or testicular injury, can increase the risk of breast cancer.
- Gynaecomastia: men with gynaecomastia (enlargement of the male breast tissue) are at increased risk of breast carcinoma. Gynaecomastia refers to development of actual breast tissue and ducts rather than just fat. The exact relationship between gynaecomastia and breast cancer is not well understood.
Progression
Because male breasts have such a small amount of breast tissue, cancer cells can quickly spread and invade surrounding structures, such as the skin or chest wall. In addition, because male breast cancer is so rare, it may be diagnosed later, when it is already locally advanced. In approximately half of cases, the lymph nodes of the axilla (armpit) are already involved at the time of diagnosis. Metastases (distant spread of cancer via the blood stream) to the lungs, brain, bone and liver are common.
Symptoms
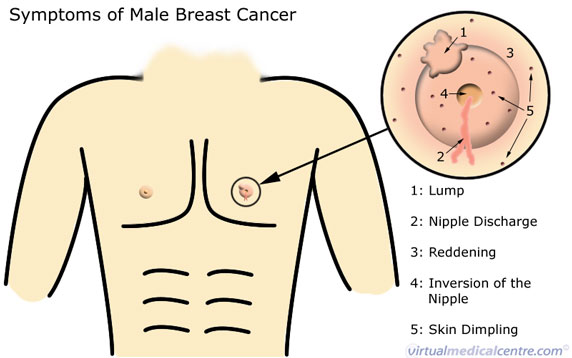
The commonest symptom of breast carcinoma is a small, painless lump in the breast. It is most often found near or under the nipple. Sometimes, a discharge from the nipple is noticed first. Other patients notice a change in the shape or appearance of the nipple or breast, experience pain in the breast, or find swollen lymph nodes in the axilla (armpit). Any changes to the size, shape or feel of the breasts should be investigated. Some common symptoms of male breast cancer are shown in the diagram below.
How is it Diagnosed
The approach to investigation of any male breast change or symptom is the same as for women; that is, the ‘triple test’ approach. This involves the following:
- Clinical history and examination: your health practitioner will ask you questions about your breast symptom, personal and family history. A clinical breast examination will examine both breasts and the lymph nodes in the axilla (armpit).
- Imaging tests with mammography or ultrasound. A mammogram is an x-ray of the breast. This may help to distinguish gynaecomastia from cancer in some men. Ultrasound may be used to examine a breast lump.
- Biopsy: this is done to sample the cells from an abnormal area of the breast. It will usually be a non-surgical biopsy; that is, a fine needle aspiration biopsy or core biopsy.
Following a diagnosis of breast cancer, blood tests including Full Blood Count and Liver Function Tests may be used to assess the possibility that the cancer may have spread to the liver or bone marrow. Other imaging tests, including chest x-rays, bone scan, abdominal CT or liver ultrasound may also be used if symptoms suggest that the cancer has spread.
Prognosis
The prognosis (outcome) of male breast cancer depends strongly on the following factors:
- Size of the tumour: larger tumours are associated with worse outcomes; and
- Lymph node involvement: cancer that has spread to lymph nodes at diagnosis has a poorer outcome than cancer which remains confined to the breast.
The general belief that male breast cancers are worse than female cancers probably stems from the fact that male breast cancer often presents at a later stage due to poor detection. However, studies have concluded that clinical outcomes for breast cancer in men are similar to those for women when they are matched for age, treatment, and stage of cancer. Overall, five-year survival rates for men with breast cancer range from 14-78%, depending on how advanced the tumour is at diagnosis.
Treatment
Most patients with breast cancer will receive a variety of treatments, which may include one or more of surgery, radiotherapy, chemotherapy and/or hormone therapies.
Surgery
If surgery is possible, male breast cancer is usually treated with a procedure called a modified radical mastectomy. This involves removal of all the breast tissue, including the nipple and surrounding areola, on the affected side. Occasionally part of the muscle under the breast will also have to be removed. The lymph nodes in the axilla (armpit) are also removed in a procedure called an ‘axillary dissection’. Sometimes, if previous tests have suggested that the cancer is at a very early stage, only one or two of the axillary lymph nodes will be removed and examined in a procedure called ‘sentinel node biopsy’. The removed lymph nodes are carefully examined for any evidence of cancer cells. If no evidence is found, the remaining lymph nodes can be left in place. Male breast cancer patients are not usually suitable for the type of breast conserving surgery sometimes used in female patients. This is because male breast cancer often involves the nipple, areola or skin, and because the amount of remaining breast tissue would be too little to conserve.
Radiotherapy
Radiotherapy may sometimes be recommended after surgery for patients with breast cancer. The aim of this treatment is to kill any remaining cancer cells which were not surgically removed, reducing the likelihood that cancer will recur. Radiotherapy usually begins 3-6 weeks after mastectomy, and lasts for 5-6 weeks. Because male breast cancer is so rare, the evidence for the use of radiotherapy in treating these cancers is not clear. Overall, however, it is thought that radiotherapy does reduce the rate of local recurrence.
Chemotherapy
Chemotherapy uses medications to target and kill any remaining breast cancer cells. Like radiotherapy, the evidence for using chemotherapy in the treatment of male breast cancer is not good. For some patients with larger cancers, or cancers that have spread, it may improve outcomes.
Hormone therapies
The majority of male breast cancers express hormone receptors (such as oestrogen receptors) on the cancer cells. These hormone receptors allow the cells to receive signals from circulating hormones like oestrogen, stimulating their growth. By targeting these hormone receptors with drugs like tamoxifen, it is possible to block the receptors and decrease the rate of cancer growth. Other drugs known as ‘aromatases’ have a similar effect by reducing the amount of oestrogen in the body. Because hormone therapies are so effective, they are recommended for use in most patients who have oestrogen-receptor positive tumours. Hormone therapies do have a number of side effects, including headaches, nausea, hot flushes, reduced libido (sex drive), or impotence. They may also increase your risk of developing blood clots such as deep vein thrombosis.
Click the links below to see for information on other breast cancers:
- Breast cancer – Adenocarcinoma of the breast
- Breast pain
- Breast cancer – Ductal carcinoma of the breast
- Breast cancer – Lobular carcinoma of the breast
- Inflammatory breast cancer
References
- Australian Institute of Health and Welfare & National Breast Cancer Centre 2006. Breast cancer in Australia: an overview, 2006. Cancer series no. 34. cat. no. CAN 29. Canberra: AIHW. [cited 28 September 2015]. Available from: [URL Link]
- Braunwald, Fauci, Kasper, Hauser, Longo, Jameson. Harrison’s Principles of Internal Medicine. 16th Edition. 2001. McGraw-Hill. [Book]
- Cotran RS, Kumar V, Collins T. Robbins. Pathological Basis of Disease. Sixth Ed. WB Saunders Company 1999. [Book]
- Giordano SH: A review of the diagnosis and management of male breast cancer. Oncologist 10 (7): 471-9, 2005. [Abstract]
- National Cancer Institute. Male Breast Cancer: Treatment [online]. U.S. National Institutes of Health. 2006. [cited 28 September 2015] Available from: [URL Link]
- Perkins G, Middleton L. Breast cancer in men. British Medical Journal. 2003; 327: 239-240. [Abstract]
- Cancer Australia. Breast cancer in men. [cited 28 September 2015Available from: [URL Link]
- National Health and Medical Research Council. Clinical practice guidelines for the management of early breast cancer. 2001. Second edition. National Breast Cancer Centre [cited 28 September 2015] Available from: [URL Link]
- Gunhan-Bilgen I et al. Male breast disease: clinical, mammographic, and ultrasonographic features. 2002. Eur J Radiol 43(3):246-55 [Abstract]
- Cancer Australia. Breast Cancer in Australia. 2015. [cited 28 September 2015]. Available from: [URL Link]
- Australian Institute of Health and Welfare. Breast Cancer in Australia: an Overview 2012. Cancer series No. 71. Cat. No. CAN67. 2012. [cited 28 September 2015]. Available from: [URL Link]
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







