- What is Pleural Effusion
- Causes of Pleural Effusion
- How do i know if i have Pleural Effusion?
- Tests
- Treatment
A pleural effusion is an excess accumulation of fluid in the pleural space around the lungs. Common causes of pleural effusion include congestive heart failure, nephrotic syndrome, pneumonia, and lung cancer. Pleural effusions may cause no symptoms at all, or may produce sharp chest pain, shortness of breath and dry cough. Treatment is aimed at the underlying cause, and symptoms can be relived by thoracentesis (draining of the fluid).
What is a pleural effusion?
A pleural effusion is an excess accumulation of fluid in the pleural space around the lungs. 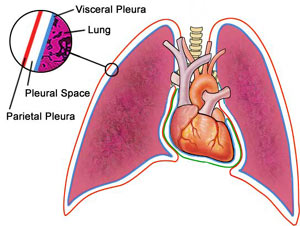
- Transudative effusions, where the excess pleural fluid is low in protein; and
- Exudative effusions, where the excess pleural fluid is high in protein.
Causes of Pleural Effusions
Anything that causes an imbalance between production and reabsorption of pleural fluid can lead to development of a pleural effusion. 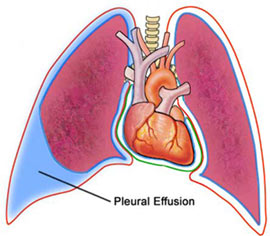
- Congestive heart failure;
- Nephrotic syndrome;
- Cirrhosis of the liver;
- Pulmonary embolism; and
- Hypothyroidism.
Exudative effusions, which are high in protein, are often more serious than transudative effusions. They are formed as a result of inflammation of the pleura, which might happen for example in lung disease. Common causes of exudative effusions include:
- Pneumonia;
- Lung cancer, or other cancers;
- Connective tissue diseases, including rheumatoid arthritis and systemic lupus erythematosus;
- Pulmonary embolism;
- Asbestosis;
- Tuberculosis; and
- Radiotherapy.
How do I know if I have a pleural effusion?
Pleural effusions may not produce any symptoms in some patients. Others may experience shortness of breath, a dry, non-productive cough, or pleuritic-type chest pain (a sharp pain, usually on breathing in, which worsens with coughing). See your doctor if you are worried about any of these symptoms. Other patients may complain of symptoms stemming from the cause of their effusion, for example swollen legs or feet in congestive heart failure. If your doctor suspects you might have a pleural effusion, he or she will ask you a number of questions to try and discover a possible cause for the effusion. This would include details of any drugs you are taking, as some medications can produce pleural effusions. Your doctor would also examine your chest and listen to your lungs with a stethoscope.
Tests for Pleural Effusion
If a pleural effusion is suspected, a chest X-Ray or chest CT can help to confirm the diagnosis. The excess accumulation of fluid can usually be seen on these images. If there is a significant effusion present on X-ray or CT, it may be necessary to take a sample of the fluid for analysis using a procedure called diagnostic thoracentesis. This involves insertion of a small needle through the skin over the pleural and into the pleural space. The fluid can then be analysed to determine whether it is transudative or exudative, depending on the amount of protein present. If the effusion is transudative, no further tests are usually necessary. This is because the cause is likely to be something systemic (affecting the whole body, for example with heart failure) and treatment can be directed towards this. If the effusion is thought to be exudative, further tests on the fluid will usually be ordered to try to identify a cause. These may include testing for presence of bacteria and examining the cell types present under a microscope to look for evidence of cancer. In approximately 15-20% of cases no cause will be found for the effusion, despite extensive investigation. Most of these cases will resolve with time.
Treatment of Pleural Effusions
If a cause for the pleural effusion can be identified, then treatment is targeted towards this cause. For example, if the effusion has resulted from congestive heart failure, diuretic therapy (fluid tablets) may be enough to clear the effusion. If no cause is found, or if the effusion is causing significant shortness of breath, therapeutic thoracentesis can be performed. This is similar to the diagnostic test described above, where a needle is inserted into the pleural space and the excess fluid drained off. If a very large amount of fluid must be drained, or if drainage needs to be continuous, then a tube can be placed through the chest wall into the pleural space (tube thoracostomy) to allow longer-term symptom relief. Rarely, some patients may require further treatment for effusions which do not resolve, or which recur despite repeated thoracentesis. They may undergo a procedure called pleurodesis (pleural sclerosis), where a chemical is injected into the pleural space to induce scarring. This scarring sticks the two layers of pleura together so that no fluid can accumulate between them.
References
- Antony, VB et al for The American Thoracic Society. ‘ATS guidelines: Management of malignant pleural effusions,’ Am J Respir Crit Care Med. 2000, 162:1987
- Braunwald, Fauci, Kasper, Hauser, Longo, Jameson. Harrison’s Principles of Internal Medicine. 16th Edition. McGraw-Hill. 2005.
- Light RW. ‘Clinical practice: Pleural effusion.’ The New England Journal of Medicine. 2002, 346(25):1971-7.
- Maskiell NA, Butland RJA. ‘BTS guidelines for the investigation of a unilateral pleural effusion in adults. Thorax. 2003, 58(suppl II):ii8-ii17
- Talley NJ, O’Connor S. Clinical Examination. 4th edition. MacLennan & Petty Pty Ltd. 2003.
- Yataco JC, Dweik RA. ‘Pleural effusions: evaluation and management.’ Cleveland Clinical journal of medicine. 2005, 72(10):854-6
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.