- What is asthma?
- Statistics on asthma
- Risk factors for asthma
- Progression of asthma
- Symptoms of asthma
- Clinical examination of asthma
- How is asthma diagnosed?
- Prognosis of asthma
- How is asthma treated?
- References
What is asthma?
Asthma is a disease of the lungs. People with asthma experience episodes of asthma, or asthma attacks. This occurs when there is a narrowing and inflammation of the airways, which makes it harder to breathe.
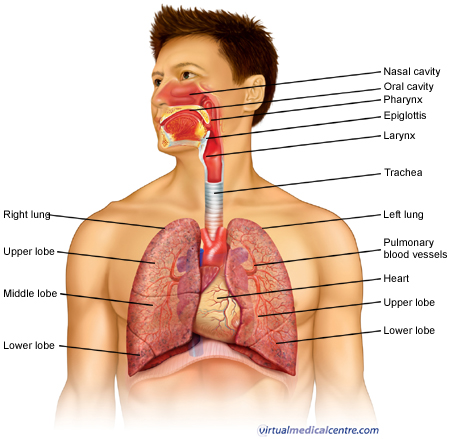
The lungs provide an interface between the air that we breathe in and the bloodstream. When a person breathes, air is drawn in through the nose and mouth and down through the trachea. The trachea divides into two bronchi, a right main bronchus and left main bronchus, to supply each lung.
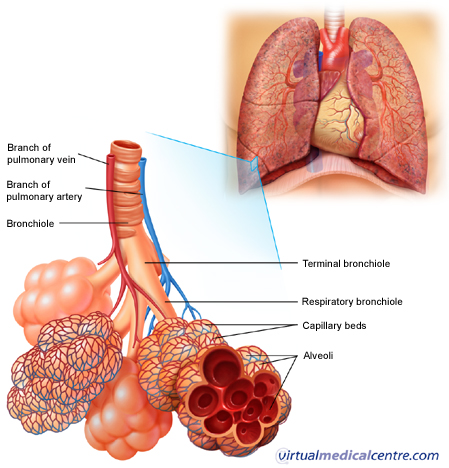
The bronchi divide into smaller bronchi, and then into bronchioles which ultimately terminate in the alveoli – the folded membranes where gas exchange takes place. The bronchi and bronchioles have a muscular layer in the wall which allows them to contract. In an acute asthma attack, this muscular layer contracts and leads to narrowing of the airways.
Inflammation may still be present between asthma attacks. This makes the airways sensitive and more likely to react to asthma triggers and cause an acute asthma attack.
 |
For more information about the respiratory system, see Anatomy of the Respiratory System. |
Asthma is sometimes divided into four main groups as follows:
- Atopic asthma: This is the most common and classic type of asthma. Patients normally have relatives who have atopic asthma, and themselves experience other allergic diseases (e.g. food allergy, eczema, hayfever). House dust mites (HDM), pollen and animal fur are common triggers.
- Non-atopic asthma: This type is triggered by respiratory infections in patients without a family history or other allergic traits.
- Drug-induced asthma: Aspirin medication can sometimes induce asthma attacks and urticaria in susceptible individuals.
- Occupational asthma: This form of asthma is induced by small quantities of chemicals and fumes, usually following repeated exposure.
Result
Bullseye - Congratulations! You have TOTAL CONTROL of your asthma. You have no symptoms and no asthma related limitations. See your doctor if this changes.
Result
On Target - Your asthma may be well controlled but not TOTALLY CONTROLLED. Your doctor may be able to help you aim for TOTAL CONTROL.
Result
Off Target - Your asthma may be poorly controlled. Your doctor can recommend an asthma action plan to help improve your asthma control.
Even if you are happy with your level of asthma control, it is important that you make an appointment with your doctor.
Statistics on asthma
Asthma is a common disease affecting more than 2.2 million Australians. Approximately 1 in every 6 children, 1 in 7 adolescents and 1 in 9 adults in Australia currently have asthma. These rates are considered high compared to the rest of the world. The worldwide number of people with asthma is increasing, especially in developed countries such as Australia.
Asthma is less common in some countries, especially in developing countries, which is probably due to a combination of genetic and environmental factors.
Children
Asthma is the most common chronic disease of children in Australia. It accounts for a significant proportion of acute hospital admissions and absent days from school. However, despite its frequency, there is no clear definition of asthma in children.
It is difficult to determine the rates of asthma in children because many children will experience symptoms of cough and wheeze which is not necessarily asthma. Doctors may be cautious in giving your child the label of asthma as this may mean other diseases of the airways may be overlooked.
Most children with wheeze will not have asthma or any significant disease. Wheeze in young children is commonly caused by viruses (e.g. cold or flu), which induce wheezing due to the immaturity of the airways.
Risk factors for asthma
The cause of asthma remains unknown. It is likely that people develop asthma as a result of a complex interaction between genes, which are inherited from your parents, and environmental factors, which are not fully understood.
One theory for this is that in developed countries we have become too clean and children are no longer exposed to enough germs, which makes them more likely to develop allergic diseases such as asthma. This theory is known in scientific circles as the Hygiene Hypothesis.
The tendency for people to be allergic is known as atopy. You are atopic if you react to allergens in tests (e.g. a skin prick test). People who are atopic may have no symptoms, or they may have symptoms of allergic disease such as eczema, hayfever or allergic asthma. It is known that people with allergies are more likely to develop asthma. 90% of children and 50% of adults with asthma are atopic.
People with a family history of asthma or allergy are more likely to develop asthma than people with no family history of asthma or allergy. Other factors that increase the risk of developing asthma include exposure to smoking during pregnancy or exposure to cigarette smoke in early childhood, and living in developed countries. Occupational asthma can result from exposure to certain chemicals and irritants at work. Research is continuing to help identify factors that cause asthma and ways to prevent asthma from developing in people who are at risk of developing asthma.
Currently the only firm recommendations to help prevent asthma in children include:
- Exclusively breastfeed your child for 6 months. If you are unable to breastfeed or don’t want to, use a partially hydrolysed formula for this period. Ask your doctor or pharmacist about appropriate brands of formula;
- Avoid smoking and smoke exposure during pregnancy and infancy.
In people with asthma, attacks can be triggered by exposure to allergens, including dust mites, animal fur (e.g. cats, dogs and horses), grass pollens, mould, viral infections such as the common cold, exposure to cold air, exercise, acute emotions such as laughter or crying, and various irritants such as chlorine bleach. The most common triggers of acute asthma attacks in children are viral infections such as the common cold.
Different people have different triggers for their asthma. What triggers asthma in one person may not trigger asthma in another person. Ask your doctor for advice on what is likely to trigger your asthma and how to avoid your triggers. Note that identification of allergens and avoidance can be difficult, particularly in children, in whom most attacks are due to viruses.
Progression of asthma
While some children do ‘grow out’ of their asthma, the tendency for sensitive airways often remains, and it is important to remain vigilant for signs of the disease re-emerging. It is often not possible to predict whether asthma is likely to get worse or better in the future, but it is known that children with allergic asthma are less likely to fully ‘grow out’ of their asthma, though it may improve with age. Children with earlier and more severe disease and a family history of asthma are more likely to find their asthma persisting into adult years.
Asthma in children is sometimes classified more specifically into three main groups:
- Infrequent episodic (intermittent) asthma: Most children (70-75%) have this type of asthma. They have only a few exacerbations per year, often associated with viral infections. In between episodes they are completely well. The asthma tends to resolve with age.
- Frequent episodic (intermittent) asthma: Children in this category (20%) have shorter intervals between exacerbations and may have 6 or more attacks per year. They may also have some mild symptoms between episodes and will benefit from preventer medications.
- Persistent asthma: These patients (5-10%) have symptoms on most days and require more intensive therapy.
Asthma can also occur for the first time in adults, where it is often not triggered by allergens. It may be work related, and symptoms triggered by allergens, chemicals or irritants in the workplace. Some people get asthma that is made worse by medications such as aspirin and other non-steroidal anti-inflammatory drugs.
Ask your doctor if you need to be careful about what painkillers you take if you are concerned that they may be triggering your asthma.
Symptoms of asthma
Asthma is characterised by acute episodes of airway narrowing, known as asthma attacks. Between asthma attacks there may be no symptoms, although many people have symptoms between attacks.
An asthma attack is characterised by coughing, wheezing, shortness of breath and chest tightness. The cough may bring up thick, yellow sputum (this does not indicate an infection). The initial attack usually occurs within 15-20 minutes of exposure to an asthmatic trigger, and subsides within an hour. This is known as the immediate asthmatic response.
In some people, a late-phase asthmatic response may also occur. This involves a more prolonged attack, occurring more than an hour after exposure to the trigger, and can last for several hours to days after exposure to the trigger.
Symptoms between asthma attacks can include night time awakenings with cough, shortness of breath, wheeze or chest tightness; early morning symptoms when you wake up; symptoms with exercise; and reduced peak flow readings.
If you have symptoms between asthma attacks, it usually indicates an element of chronic airways inflammation. These people usually respond well to preventative medications such as inhaled glucocorticosteroids.
When you see a doctor complaining of symptoms of cough or wheeze, your doctor will try to determine the exact pattern of symptoms and likely triggers. It is also important to find out whether any one else in your family suffers from asthma or any other related diseases (e.g. hayfever). A history of these conditions in yourself also supports the diagnosis of asthma.
Children
Diagnosis of asthma is much more difficult in children due to the wide variety of other conditions that can cause similar symptoms. In general, children with asthma will have recurrent and persistent wheezing. Your doctor will take a detailed history to exclude other causes such as:
- Transient infant wheezing: In this case your child may have started wheezing in infancy due to exposure to cigarette smoke. However, nobody else in the family has asthma or atopic disease, so asthma is unlikely.
- Cystic fibrosis: This is an inherited disease that disturbs mucous production and secretion throughout the entire body. Children may have recurrent chest infections and associated poor growth rate or weight gain.
- Inhaled foreign bodies: This diagnosis is suggested if your child has a sudden onset of wheezing, perhaps associated with a coughing or choking episode.
- Structural abnormalities of the airways: Onset of symptoms at birth.
- Heart failure: Due to congenital heart disease.
As with adults it is als important to obtain a detailed personal and family history of atopy.
Clinical examination of asthma
Between asthma attacks there are often no signs of asthma. Your doctor will thoroughly examine your respiratory system, particularly looking for evidence of wheeze or hyperexpanded lungs. Your doctor may also find evidence of allergic disease (e.g. eczema or hayfever), or you may have reduced lung function.
If you are having an acute asthma attack, your doctor may find the following signs:
- Wheezing;
- Tachypnoea (fast breathing);
- Tachycardia (fast heart rate);
- Prolonged expiration (takes longer to blow out all of the air in your lungs);
- Prolonged forced expiratory time (decreased peak flow, decreased FEV1);
- Use of accessory muscles of respiration (because it is harder to breathe);
- Hyperinflated lungs (may be seen on chest x-ray or recognised because the liver is pushed down).
Signs of more severe asthma include:
- Appearance of exhaustion and fear;
- Inability to speak because of breathlessness;
- Drowsiness;
- Very rapid heart beat;
- Cyanosis (blue lips);
- Reduced oxygen saturation of the blood: This is measured by a clip placed on the end of your finger;
- Reduced breath sounds heard by the doctor.
How is asthma diagnosed?
Your doctor may order the following investigations to help diagnose asthma.
Blood tests
While there are no blood tests that can be done to diagnose asthma, some can help determine whether you have an allergic tendency (such as total IgE measurements) or can help your doctor decide which treatment is most appropriate.
RAST tests look at the blood’s response to certain allergens and can help determine what you are allergic to.
Your full blood count may show raised level of eosinophils, which occurs in asthma and other allergic conditions.
Chest x-ray
Again, this investigation does not diagnose asthma, but a chest x-ray may be useful to exclude other causes of symptoms (e.g. pneumothorax), or to detect a rare cause of asthma (e.g. allergic bronchopulmonary aspergillosis).
Spirometry
Spirometry and other lung function tests are the main diagnostic tools in asthma. Spirometry measures the volume breathed in and out during inspiration and expiration, and can help your doctor determine whether there is obstruction.
Your doctor will test your lung function before and after taking a bronchodilator medication. If your lung function improves, it is highly suggestive of asthma.
Another measurement, called peak expiratory flow rate (PEFR), is useful for monitoring your lung function over time and demonstrating the variability in lung function that is characteristic of asthma.
Exercise tests
Some patients only experience asthma symptoms during exercise. Your doctor may perform spirometry before and after you do exercise. This can help diagnose exercise-induced asthma.
Lung provocation tests
Very rarely, your doctor may perform a test that involves you inhaling small amounts of histamine or methacholine, then taking measurements of your lung function periodically with spirometry.
The theory behind this test is that patients with asthma have hyper-reactive airways, so small doses of these agents can lead to constriction of the airways. A reduction of lung function with increasing doses of these agents supports the diagnosis of asthma. This test is usually only done if spirometry doesn’t produce sufficient results.
Skin prick tests
Skin prick testing involves making several small pricks to the skin of the arm, and introducing small amounts of common allergens. The wheal which occurs over each site is an immune reaction; a large or long-lasting wheal indicates a hypersensitivity to the allergen. This may identify allergic asthma triggers.
Common allergens tested for by skin prick tests include dust mite, cat, dog, grass pollens and mould.
Investigating asthma in children
Diagnosis of asthma in children is much more difficult. Unfortunately for young children, there is no definitive test to diagnose asthma. Only children older than 6 or 7 are able to adequately perform spirometry or peak expiratory flow rate to produce reliable measurements of lung function. If your child is less than this age, it may mean your doctor cannot definitively say whether your child does or does not have asthma, which may be frustrating for you.
In younger children, your doctor can try giving bronchodilator medications and seeing if there is a detectable clinical response. They can also perform some of the allergy tests described above, such as RAST or skin prick tests, to determine whether your child has an allergic tendency. However, these tests are not reliable in children less than 2 years old, as results can change over time as the immune system matures. Furthermore, while atopy supports the diagnosis of asthma, it does not give a definite answer.
Prognosis of asthma
There are a large number of people who live with asthma, many of whom are able to gain good control with no symptoms from day to day. Asthma should not prevent you from leading a fulfilling life or stop you from competing actively in sports and other hobbies.
However, you should remember that asthma can be a potentially fatal disease and it is important to have your asthma regularly reviewed by your doctor, even when you are well. Figures show that approximately 300 Australians die from asthma attacks per year, many of which are preventable. Adults especially can become lazy about adhering to their management, so make sure you are always vigilant and adhere to your personal action plan. Your doctor will be able to provide support and advice for you to achieve this.
People with asthma who are at risk of severe asthma attacks include:
- Previous hospital admission, especially to the intensive care unit;
- Hospital admission in last 6 months;
- Excessive use of reliever puffers such as Ventolin;
- Long-term oral steroid treatment (required for people with very severe asthma);
- Patients who are not using preventers or who do not take their puffers regularly as prescribed;
- Night-time attacks or symptoms that are worse in the morning;
- Recent stressful life-events and strong emotional expression (e.g. laughter, crying);
- Patients who do not recognise when their asthma is getting worse.
You and your doctor should work together as a team to devise a personal management plan and recognise when your symptoms are becoming worse.
How is asthma treated?
Asthma management involves more than just simple medications. It relies on education of the patient and family as well as lifestyle changes involving diet, smoking cessation and exercise. Your doctor will try to devise a management plan which allows you to:
- Achieve as normal a lifestyle as possible, including a normal exercise tolerance;
- Avoid night-time awakenings due to asthma;
- Avoid exacerbations;
- Avoid important adverse effects from treatment.
The treatment of asthma in Australia is centered around the 6 Step Asthma Management Plan developed by the National Asthma Council.
- Assess the severity of the asthma.This can be done using spirometry or other lung function tests and by looking at the effect of asthma on your daily life. Your doctor may describe your asthma as mild, moderate or severe depending on your frequency of symptoms, lung function, hospital admissions and requirement for medications.
- Achieve best lung function.This involves finding the right medications for optimal lung function and to minimise day to day symptoms. Medications are often started at high doses to bring the asthma under control, and then the doses will be reduced to avoid side effects.
- Identify and avoid trigger factors.If you know what triggers your asthma, you can take measures to reduce your exposure to your triggers (e.g. pets, cigarette smoke, or dust). Allergen avoidance can be difficult, as your asthma may have multiple triggers.
- Maintain best lung function with optimal medication.A long-term medication program is planned and monitored by repeat lung function measurements and asthma symptoms. This will usually involve both “reliever” and “preventer” medications designed to minimise potential side effects.
- Know your action plan.An action plan is prepared with your doctor, and involves how to recognise when your asthma is getting worse, what to do when your asthma is getting worse, and when you should seek medical help.
- Check your asthma regularly.It is important to have regular asthma reviews by your doctor, even when your asthma is under control or not very severe. During these reviews, your doctor will measure your lung function, discuss recent symptoms, review medications and check your inhaler technique.
Medications for asthma
Medications for asthma include relievers, preventers and symptom controllers.
Relievers
Reliever medications are usually inhaled from puffers (with or without a spacer), and are bronchodilators, meaning they act immediately by relaxing muscles surrounding the airways of the lung.
Reliever medications are taken when an asthma attack happens, and before exercise to prevent attacks in those suffering from exercise-induced asthma. Pharmacological classes of bronchodilator include B2 receptor agonists (e.g. Ventolin and Bricanyl), ipratropium bromide (e.g. Atrovent), and methylxanthines (e.g. tablets such as Brondecon and Theodur).
Reliever medications may also be taken by nebuliser, in which a solution of the medication is converted to a mist of small droplets by a flow of oxygen or air through the solution. This mist is then inhaled.
Preventers
Preventer medications are directed at preventing the bronchial hyper-reactivity and airway inflammation that occurs in asthmatics. Pharmacological classes include corticosteroids, cromones and leukotriene receptor antagonists.
Corticosteroids are very common and very effective preventer medications, and include Q-VAR, Pulmicort, Flixotide and Alvesco. They are taken regularly, irrespective of asthma symptoms, usually by puffer. Side effects include oral thrush, hoarse voice, cough and, occasionally, adrenal gland suppression (causing hormonal imbalance). Corticosteroid tablets (oral) are given as preventers to some patients with severe chronic asthma, but are usually only used in the treatment of severe asthma attacks.
Cromones include Intal, Intal forte, and Tilade. They are inhaled from a puffer and side-effects are less common. The puffers need to be cleaned daily.
Leukotriene receptor antagonists include Singulair and Accolate, and are taken as tablets. They are commonly used in children with less severe asthma. Side effects are less common than with corticosteroids.
Symptom controllers
Symptom controllers are long-acting relievers such as Oxis and Serevent. These are taken as puffers once or twice a day for people who still have symptoms when taking regular preventers. Symptom controllers can allow people with more severe asthma to reduce their steroid dose (and hence minimise side effects) without causing more symptoms of asthma to appear.
Using puffers
As most asthma medications are taken by puffers, it is very important to use the correct technique. At least one third of puffer users do not use their puffer correctly. This means that medication does not reach the lungs, and has a substandard effect.
The most effective way to deliver medication via a puffer (metered dose inhaler or MDI) is in combination with a large volume spacer such as a Volumatic. This is a device that attaches to the puffer and allows more medication to be delivered to the lungs.
To use your puffer and spacer
- Remove the cap. Shake the puffer vigorously for 1-2 seconds. Attach the puffer to the spacer.
- Slowly blow out to a comfortable level. Close your lips around the mouthpiece of the spacer.
- Press the puffer firmly, once. Breathe in through your mouth as deeply as possible over 3-5 seconds (do not breathe in through your nose).
- Hold your breath for about 10 seconds; then breathe out gently.
- Breathe normally for about one minute, then repeat the inhalation.
Spacers are so effective at delivering medication that they are often used in emergency departments for acute asthma attacks instead of nebulisers, as studies have shown that they are at least as effective as nebulisers and are less expensive.
If a spacer is not available, the following technique is suitable for adults and children over the age of seven.
To use your puffer
- Remove the cap. Shake the puffer vigorously for 1-2 seconds. Hold it upright (canister on the top).
- Hold the mouthpiece of the puffer 4-5 cm away from your mouth.
- Tilt your head back slightly with your chin up. Open your mouth and keep it open.
- Slowly blow out to a comfortable level. Close your lips around the mouthpiece.
- Just as you start to breathe in (slowly) through your mouth, press the puffer firmly, once. Breath in as far as you can over 3-5 seconds (do not breathe in through your nose).
- Close your mouth and hold your breath for about 10 seconds; then breathe out gently.
- Breathe normally for about one minute, then repeat the inhalation.
Other devices used to deliver medication to the lungs include the Autohaler (a breath-activated MDI), Turbuhaler, Accuhaler, Diskhaler and Rotahaler.
Turbuhalers and Accuhalers are widely used as an alternative to MDIs. These are breath-activated devices which deliver medication in dry powder form and do not require a spacer.
Simply prime the puffer as shown in the instruction leaflet, then breathe deeply over 3-5 seconds through your mouth and hold your breath for about 10 seconds before breathing out.
Management of asthma in children
Management of asthma in children follows the same general principles as management in adults, but there are some important differences due to variations in the severity, pattern and natural history of the disease, and potential for side effects in children.
Like adults, a similar 6-step asthma management plan should be followed which involves regular review and follow-up. It is also important that you understand the difference between preventer and reliever medications.
Preventer medications should be taken every day as they inhibit underlying inflammation. Reliever medications are used to treat acute attacks.
The majority of children have only mild infrequent episodic asthma. Most of these children can be managed with a bronchodilator medication as required. However, if your child has recurrent asthma symptoms, your doctor will need to start an anti-inflammatory medication. Children are more susceptible to the side effects of long-term medications, so care must be taken to find the lowest effective dose.
Children with frequent intermittent or mild persistent asthma are often prescribed one of three classes of medications: inhaled cromones, oral leukotriene receptor antagonists, or low dose inhaled corticosteroids. The former are particularly effective for exercise-induced asthma in children, but are rarely used in adults. Children with more severe persistent asthma are usually managed with steroids.
Coordinating the inhaler technique is often difficult for children. It is therefore very important that children use their puffers in conjunction with a spacer device to ensure enough medication gets in the lungs. This also avoids local side effects from steroid preventers (e.g. oral thrush or hoarse voice).
Children younger than 5 years should use a small volume spacer. Those above 5 should start on a large volume (adult) spacer as their lungs take in a greater volume of air. Children younger than 3 years should use a mask in conjunction with their spacer.
Your doctor will demonstrate how to use these devices. Children using a large volume spacer use the same technique described above. Those using the smaller spacers should take 5 deep breaths in and out following each puff.
Acute asthma attacks
Acute attacks of asthma may require hospital admission. Here the doctors will administer regular bronchodilator medications such as salbutamol (Ventolin) and ipratropium (Atrovent). These are usually given via a puffer and spacer, but are occasionally given via a nebuliser machine. You will also be administered oxygen and be closely monitored.
Most adults and children will be given a short course of oral steroids following the acute attack. In very severe attacks it may be necessary for you to be intubated, ventilated or sent to ICU.
Appropriate follow-up is essential to review medications, triggers and your asthma plan, in order to avoid future severe attacks.
Please go to our Supportive Care section for doctor accredited support and public awareness groups on asthma.
More information
 |
For everything you need to know about what to do in an asthma attack, correct inhaler techniques, written asthma action plans and other useful resources, visit Asthma. |
References
- Australian Government Department of Health and Ageing. Asthma and allergy: A guide for health professionals [online]. South Melbourne, VIC: National Asthma Council Australia; 2005 [cited 22 February 2007].
- Chipps BE. Determinants of asthma and its clinical course. Ann Allergy Asthma Immunol. 2004;93(4):309-16. Available from: [Abstract]
- Cotran RS, Kumar V, Collins T, Robbins SL. Robbins Pathologic Basis of Disease (6th edition). Philadelphia: WB Saunders Company; 1999. Available from: [Book]
- Guilbert T, Krawiec M. Natural history of asthma. Pediatr Clin North Am. 2003;50(3):523-38. Available from: [Abstract]
- Landau L. Early childhood asthma: What we know and what we need to know. Definitions and early natural history. Med J Aust. 200;1777(6 Suppl):S38-9. Available from: [Abstract]
- Le Souëf PN. Early childhood asthma: What we know and what we need to know. Risk factors and epidemiology. Med J Aust. 200;1777(6 Suppl): S40-1. [Abstract]
- Asthma management handbook 2006 [online] South Melbourne, VIC: National Asthma Council Australia; 2005 [cited 22 February 2007]. Available from: [URL link]
- Asthma death toll steadies [online]. South Melbourne, VIC: National Asthma Council Australia; 8 December 2005 [cited 22 February 2007].
- Robinson MJ, Robertson D (eds). Practical Paediatrics (5th edition). Sydney, NSW: Churchill Livingstone; 2003.
- Tang ML. Early childhood asthma: What we know and what we need to know. Is prevention of childhood asthma possible? Allergens, infections and animals. Med J Aust. 200;177(6 Suppl):S75-7. Available from: [Abstract]
- Tattersfield AE, Knox AJ, Britton JR, Hall IP. Asthma. Lancet. 2002;360(9342):1313-22. Available from: [Abstract]
- Zangger J, Hall E. Asthma and wheezing in the first years of life: A guide for health professionals [online]. South Melbourne, VIC: National Asthma Council Australia; 2005 [cited 22 February 2007].
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.