- What is giant papillary conjunctivitis (GPC)?
- Statistics of GPC
- Risk factors for GPC
- Progression of GPC
- Symptoms of GPC
- Clinical examination of GPC
- How is GPC diagnosed?
- Prognosis of GPC
- Treatment of GPC
- GPC prevention
- References
What is giant papillary conjunctivitis (GPC)?
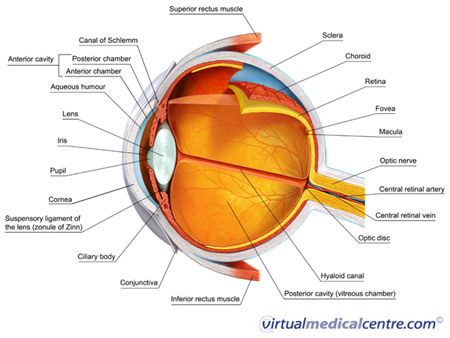
Conjunctivitis is a very common reason for experiencing an uncomfortable red eye. There are a number of causes for conjunctivitis, including bacteria, viruses and, importantly, allergies. Allergic conjunctivitis affects the conjunctiva of the eye. The conjunctiva refers to the thin, translucent lining of the eyeball and the undersurface of the eyelids.
Giant papillary conjunctivitis (GPC) is a type of allergic conjunctivitis. In GPC, a foreign body causes prolonged mechanical irritation, which results in a reaction in the eye. Most commonly, contact lenses are the foreign body causing the irritation.
Statistics of GPC
The rate of GPC in contact lens wearers is about 21%, but this may range from 4% to 36% depending on how often the contact lens are replaced. The condition is experienced most by those who wear soft contact lenses, while only about 1–5% of those who wear hard contact lenses are affected.
Risk factors for GPC

As GPC represents a reaction in response to foreign body irritating the eye, factors such as the use of contact lenses, recent eye surgery involving sutures (stitches), and having an artificial eye lens are all associated with the development of GPC.
There is evidence that the development of GPC is influenced by how often contact lenses are changed. Contact lens wearers who replace their lenses more frequently appear less likely to develop GPC than those who replace their lenses less often.
Symptoms of GPC
It is important that anyone with eye symptoms visits their doctor and provides a detailed clinical history. The doctor will rule out other types of conjunctivitis and more serious conditions that may cause uncomfortable red eyes.
Most people affected with GPC will experience tearing, itching and redness in their eyes. Early on in the condition, you may experience mucous discharge, particularly in the morning. There may also be itching of the eyes when the contact lenses are removed. As the condition progresses, you may experience a foreign body sensation, eye discomfort, and find that you can only tolerate wearing your contact lenses for a short period of time. Some people may experience blurred vision due to mucus covering the contact lens.
The doctor will pay close attention to several aspects of your clinical history. In particular, they may ask:
- Have you had recent exposure to other people with conjunctivitis or an upper respiratory tract infection? This may suggest a viral cause of conjunctivitis.
- What are the details of your sexual history? In particular, have you had chlamydia or gonorrhoea? These can both cause conjunctivitis.
- Are you using any prescription or over-the-counter medications? Some medications can cause inflammation.
- Have you had any eye diseases before, used contact lenses, or had any other conditions that can be associated with eye conditions (e.g. rheumatoid arthritis)?
- Has anyone in your family had allergic conditions (e.g. hayfever, asthma or eczema)?
A different type of conjunctivitis, vernal keratoconjunctivits (VKC), may have similar symptoms to GPC. Therefore a vital question the doctor will ask is whether you wear contact lenses, as this is a key feature in the history of GPC.
If you experience severe, continuous eye pain and reduced vision, you must see your doctor quickly and you may need urgent referral to an ophthalmologist. These features are not typically present in allergic conjunctivitis and may point to a more serious eye condition.
Clinical examination of GPC

The doctor may also use an ophthalmoscope to view the back of your eye, or a slit-lamp microscope to see the front structures of your eye. Both of these are painless, routine examinations.
How is GPC diagnosed?
Investigations are not usually required, as the diagnosis of GPC can be made on the basis of the clinical history and examination.
Prognosis of GPC
The prognosis for GPC is generally favourable and permanent visual loss is not experienced. Ceasing contact lens use improves the symptoms. Over 90% of people will be able to tolerate contact lenses again, provided measures such as frequent lens replacement, swapping to rigid contact lenses, improved cleaning regimes and topical anti-inflammatory medications are used.
Treatment of GPC

GPC due to contact lens use often requires changing the contact lens routine and reducing the wearing time to a just few hours a day. Switching to daily disposable lenses is helpful for more persistent cases of GPC. In more severe cases that do not respond to these measures, it may be necessary to stop wearing the contact lenses for a time.
Mast cell stabilisers
Topical mast cell stabilisers can help some people with GPC. Mast cells play an important role in allergic conjunctivitis. Mast cell stabilisers prevent mast cells from opening up and releasing histamine and other chemicals that produce the symptoms seen in GPC. Mast cell stabilisers do not relieve the immediate symptoms, but control the long-term signs and symptoms of GPC.
This medication should not be used at the same time that contact lenses are worn; it should be used before and after lens insertion and removal. Mast cell stabilisers are effective in most people and are generally safe but, like all medications, they should only be used according to your doctor’s advice.
NSAIDS
NSAIDs may be used to treat certain cases of GPC, although they are not commonly used.Topical NSAIDs reduce the itchiness and redness associated with GPC by blocking the enzymes involved in producing the chemicals that contribute to allergy and inflammation. If NSAIDs are prescribed for GPC, a course of 2–4 weeks generally produces some improvement in the signs and symptoms.Significant side effects can occur with NSAID use, so keep your doctor updated on how your treatment is progressing.
Steroids
Steroids may treat some cases of GPC and can reduce the inflammation and redness of the eyes. When using steroids, you need to be regularly reviewed by your doctor due to the possible side effects, including glaucoma, cataracts and eye infections.
Immunomodulating agents
Some people with GPC may find immunomodulating agents to be helpful. Cyclosporin is one medication within this group. Cyclosporin attaches itself to certain cells in the body, known as T-lymphocytes. By binding to these cells, cyclosporin prevents the production of chemicals involved in inflammation, and therefore reduces inflammatory and allergic symptoms. In patients with GPC, removing the foreign body and using either topical or systemic cyclosporin agents usually has a positive response. Immunomodulating agents are powerful medications and should be used with caution and only following the instructions of your doctor.
If you find your symptoms are not improving or are getting worse despite treatment, you should return to your doctor as soon as possible for a review.
GPC prevention
Some useful strategies for avoiding GPC due to contact lens use include:
- Take care not to over-wear the lenses;
- Dispose of the lenses in the advised time frame; and
- Maintain a high standard of contact lens care.
More information
 |
For more information about allergic conjunctivitis and its subtypes, see Allergic Conjunctivitis. |
References
-
Khaw PT, Shah P, Elkington AR. ABC of Eyes (4th edition). London: BMJ Publishing Group; 2004.
-
Bielory L, Friedlaender MH. Allergic conjunctivitis. Immunol Allergy Clin North Am. 2008;28(1):43-58. [Abstract]
-
Khurana AK. Comprehensive Ophthalmology (4th edition). New Delhi: New Age International Publishers; 2007.
-
Moloney G, McCluskey PJ. Classifying and managing allergic conjunctivitis. Medicine Today. 2007;8(11):16-21. [Full text]
-
Porazinski AD, Donshik PC. Giant papillary conjunctivitis in frequent replacement contact lens wearers: A retrospective study. CLAO J. 1999;25(3):142-7. [Abstract]
-
Reinhard T, Larkin DFP (eds). Cornea and External Eye Disease. Heidelberg, Germany: Springer-Verlag; 2006.
-
Bartlett JD, Jaanus SD. Clinical Ocular Pharmacology (5th edition). Boston: Butterworth-Heinemann; 2008.
-
Smolin G, Foster CS, Azar DT, Dohlman CH (eds). The Cornea: Scientific Foundations and Clinical Practice (4th edition). Philadelphia: Lippincott Williams and Wilkins; 2005.
-
Krachmer JH, Mannis MJ, Holland EJ (eds). Cornea (2nd edition). China: Elsevier Mosby; 2005.
-
Bennett ES, Weissman BA. Clinical Contact Lens Practice. Philadelphia: Lippincott Williams & Wilkins; 2005.
-
Schmid KL, Schmid LM. Ocular allergy: Causes and therapeutic options. Clin Exp Optom. 2000;83(5):257-270. [Abstract]
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







