- What is Renal Failure – Acute
- Statistics on Renal Failure – Acute
- Risk Factors for Renal Failure – Acute
- Progression of Renal Failure – Acute
- Symptoms of Renal Failure – Acute
- Clinical Examination of Renal Failure – Acute
- How is Renal Failure – Acute Diagnosed?
- How is Renal Failure – Acute Treated?
- Renal Failure – Acute References
What is Renal Failure – Acute
Your kidneys are two very important organs in the body, which help perform many functions. Some of these functions include: helping you get rid of waste products, forming urine, controlling levels of important molecules such as sodium, potassium and chloride, and producing hormones that stimulate the production of red blood cells when the oxygen carrying capacity of the blood is not optimized.
Acute failure of the kidneys is a condition in which there is a rapid loss of the normal function of your kidneys, due to a sudden, acute or chronic insult. This means that they can not perform their normal functions, resulting in a range of complications. Some of these include: the build up of waste products that the kidneys usually excrete, such as urea and creatinine, high or low concentrations of molecules such as sodium and potassium, low numbers of red blood cells, inability to concentrate the urine properly and build up of excess fluid. Acute kidney failure should be treated as a serious condition and is a potential medical emergency.
Statistics on Renal Failure – Acute
Acute failure of the kidneys is not a rare condition, with the incidence depending on the definition used and the population studied. People who are hospitalized in hospital intensive care units (ICUs) are at very high risk for acute kidney failure. A large multinational study was recently published in 2005, which studied over 29000 ICU patients in multiple countries to try and determine the incidence of acute kidney failure. Patients were studied from September 2000 to December 2001 in 54 hospitals in 23 countries, including Australian medical centres and hospitals such as: Austin and Repatriation Medical Centre, Western Hospital, Sir Charles Gairdner Hospital, Frankston Hospital and Flinders Medical Centre. Of the 29 269 critically ill patients admitted during the study period, approximately 6% developed acute renal failure during their ICU stay.
The incidence of kidney disease due to bacteria such as streptococci has been gradually decreasing with the increasing living standards in Australia. However, in many Indigenous communities, high incidences of streptococcal infection and kidney disease are still seen. It is estimated that the Indigenous population have a ten times greater risk of eventually developing renal failure after they have had bacterial infections, than compared to the non-Indigenous population.
Risk Factors for Renal Failure – Acute
The most common causes of acute kidney failure are those conditions that cause reduced blood supply to the kidneys. Poor blood supply to the kidney leads to abnormal kidney function.
Generally, causes of acute kidney failure can be divided into three groups – pre-renal (ie affecting the body’s volume and vessels supplying the kidneys, renal (within the kidney) and post renal (affecting pathways and structures after the kidneys).
Examples of these groups of causes include:
Pre-renal (often due to decreases in the blood supply):
- Low blood pressure (Hypotension), from causes such as dehydration, fluid loss and shock.
- A decrease in blood volume due to: bleeding, vomiting, diarrhoea, decreased intake, burns, sepsis, liver disease , malnutrition.
- Problems with the vessels such as build up of fat and clots in arteries (atheroembolic disease), and occlusion of the renal artery.
- Reduced output from the heart, due to causes such as – myocardial infarction (heart attack), heart failure, pulmonary embolus(a clot in the lungs), dysfunction of the heart valves.
Renal (damage to the kidney itself):
- Infections – to the kidney itself, or within the bloodstream (eg sepsis).
- Toxic medications or contrast – eg aminoglycoside antibiotics, non-steroidal anti-inflammatory drugs, tetracyclines, iodine contrast. As the kidneys are one of the primary means that the body excretes drugs and drug by-products, they are susceptible to damage induced by medications such as those listed above. Toxic medications, infections and decreased blood supply to the kidneys are some of the insults that can contribute to one of the most common causes of kidney failure; acute tubular necrosis – destruction and death of the tubules within the kidneys.
- Acute disease of the kidneys (acute glomerulonephritis) due to: immune causes, development of antibodies and sometimes from unknown causes.
- Rhabdomyolysis (breakdown of muscle tissue) – muscles can be damaged by factors such as: injury, medications including statins (used to help lower cholesterol levels) and prolonged inactivity. This results in the release of myoglobin in the blood, which can affect the kidneys.
- Haemolysis (breakdown of red blood cells) – this releases haemoglobin, which damages the kidneys tubules and can be due to conditions such as sickle cell disease, vasculitis and haemolytic uraemic syndrome .
Post-renal (obstruction in other parts of the urinary tract) such as:
- Obstruction of the urethra/ureters by stones, clots or other debri.
- Abnormalities in the bladder wall such as strictures and the muscles in the bladder not contracting properly.
- Abnormalities outside the urinary tract, but which result in compression of parts of the urinary system such as tumours (eg ovarian, colorectal, prostate cancer).
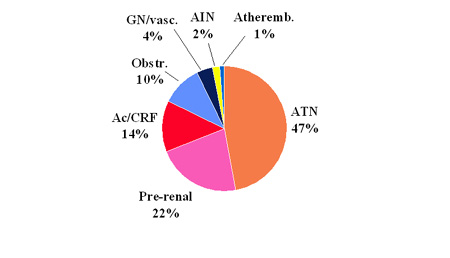
Image courtesy of Mark Thomas
Progression of Renal Failure – Acute
The prognosis of patients with kidney failure depend primarily upon the underlying cause and presence or absence of other medical conditions. With progression of time, the mortality has decreased, due to better understanding of the causes and optimal treatment. In cases where the cause is pre-renal or post renal, the kidneys often show a good recovery once the precipitating factor is removed.
There is a higher mortality rate that is seen especially in surgical and trauma patients. In patients who are in intensive care units, there is an estimated mortality rate of 50% or more. This is often due to the underlying disease and other existing medical conditions rather than to complications of kidney failure alone.
If you have established kidney failure, complications due to accumulation of waste products and fluids may occur in the next few days. After two – four days, high levels of calcium, phosphate and potassium may develop. Five to seven days later, you may experience symptoms from excessive build up of urea including – drowsiness, hiccups, nausea, easy bruising, bleeding and itching. End stage complications (which should be prevented from occurring) include: abnormalities of the heart rhythm, build up of fluid in the lungs and bleeding into the space around the heart and the gut.
In the longer term, the results vary depending on the underlying cause of the kidney failure. Recovery from ARF usually starts between 7 and 21 days of its onset in surviving patients. In some cases, it is thought that there may be progressive worsening and dysfunction of the kidneys after an episode of acute kidney failure. Acute kidney failure is irreversible in approximately 5% of patients, increasing to 16% in elderly patients. In children, episodes of kidney failure may leave them prone to developing kidney problems later in adolescence or adulthood.
Symptoms of Renal Failure – Acute
Your medical practitioner may ask certain questions to help determine the cause of your kidney failure and help guide optimal management of your kidneys. The cause of renal failure can often be determined by obtaining a good history. One of the most important questions to answer is whether you are still producing urine. If you are not still producing urine, this is a medical emergency and requires more aggressive management.
To help determine whether the cause of your kidney failure is acute or chronic, the doctor will often ask if you have had any previous problems or investigations of the kidneys, and whether you have had any blood tests to assess the function of the kidneys.
Further questioning can be directed towards identifying the specific cause of your kidney failure:
- Fluid loss – have you experienced any major losses of fluids – ie dehydration, vomiting, diarrhoea, been taking fluid tablets, burns, etc.
- Medications – have you been taking any medications that may damage your kidneys or started on any new medications recently? These medications include anti-inflammatories, some antibiotics and blood pressure tablets.
- Have you noticed any changes in your urine – eg blood, pain, frothing, poor urinary stream, difficulty passing urine, a decrease or increase in the amount of urine produced, dribbling.
- Have you experienced any symptoms suggestive of longer standing kidney failure in the past – fatigue, weakness, loss of weight and appetite, vomiting, shortness of breath, bruising, itching, bone pain.
Clinical Examination of Renal Failure – Acute
When the doctor examines you, he or she may concentrate on the following areas:
Fluid Balance of The Body
To accurately assess how much fluid is in the body, your urine output, blood pressure (lying and standing) and pulsations of veins in your neck may be used. If you are producing minimal amounts of urine, have low blood pressure, an increased heart rate and dry skin and mucous membranes, this suggests a state of volume depletion / insufficiency. Signs of too much water retention in the body often do not manifest until you have gained more than 2 kg in water.
Your heart and lungs may also be examined – any signs of heart failure or severe hypertension (high blood pressure) can contribute to worsening of the kidney’s function.
There may also be signs specific to underlying disease processes – ie signs of infection, systemic symptoms and findings suggestive of concurrent diseases such as inflammation of the vessels (vasculitis: fever, skin rash, joint pains, lesions in the lungs), chronic kidney failure (high blood pressure, build up of fluid, bruising, scratch marks).
Causes of post renal failure may also manifest clinically. You may have an enlarged bladder which can be felt on examination, or a mass in the abdomen that is discovered. Pain on the left or right sides of the lower abdomen may suggest a kidney stone, infection or obstruction.
How is Renal Failure – Acute Diagnosed?
There are various tests that can be used to help the doctor diagnose a problem with
your kidneys and assess the degree of kidney failure present. These include:
- Bloods – With the onset of kidney failure, blood tests will be required frequently to assess renal function and to also to help determine the cause of the kidney failure. This blood is usually taken via a small needle inserted into one of the veins in your arms. A blood test can also be performed on blood taken from your arteries, to determine the levels of oxygen and other ions and electrolytes in the blood. This is usually done if you are admitted to hospital and are acutely unwell.
- Urinalysis – Urine tests can also be performed to help determine the cause of your kidney failure. A sample of urine is tested with a stick that measures the levels of blood, glucose, protein and presence of other substances, and also sent off to the laboratories to be tested. The technician or doctor reviewing the urine will look at the sample under a microscope and also see if any organisms can be grown from the sample.
- Electrocardiogram (ECG) – An ECG (measure of the electrical activity within the heart) may also be required on a number of occasions to detect abnormal heart rhythms that can be caused by kidney failure.
- Radiology / Imaging – Imaging techniques such as ultrasound may identify small, shrunken kidneys, which is consistent with chronic, long standing disease. The presence of obstruction in the urinary system, kidney stones or other masses can also be identified.A chest x-ray may also be required if breathing becomes difficult, as fluid may collect in the lungs in many cases.
- In a small number of cases, where other investigations have failed to determine the cause of your kidney failure, a biopsy (sample of tissue) from the kidneys may be taken.
- There is also a measurement known as the Glomerular Filtration Rate (GFR), which is the rate at which the kidney filters fluids. The GFR provides us with an idea of the underlying function of the kidney. A decrease in the GFR can be due to progression of kidney failure or due to a superimposed insult to the kidneys, such as decreased blood flow to the kidneys from dehydration or blood loss. An increase in the GFR is often a good thing, reflecting an improvement in kidney function.The GFR is less accurate in certain groups of patients, such as children, pregnant women and those people with increased muscle mass and weight (eg obese patients, body builders).The trend in your GFR is useful in providing the doctor with an idea of the progression and improvement or deterioration of your kidney function.
How is Renal Failure – Acute Treated?
The main objectives in the treatment of kidney failure include the treatment of underlying causes and provision of support through the acute kidney failure to recovery. There are both pharmacological (medical) and non-pharmacological (supportive) measures that can be employed in treating kidney failure.
Management can be broken down into three major areas:
-
- General Measures
Fluid and electrolyte balance will need to be closely monitored to prevent the complications of ARF. This may require close monitoring of urine output and multiple blood tests throughout the day and night. Any drugs that could be harmful to the kidney (eg blood pressure medications such as ACE inhibitors, digoxin, amphotericin, aminoglycosides) are stopped. Any contrast or radiological dyes are avoided especially in the short-term. - Fluid and Electrolyte balance
If you show any signs of dehydration or have experienced any loss of fluid from the body, the doctor will provide you with adequate fluids via your veins into your body and also encourage oral intake of fluids. This replacement is guided by your vital signs (heart rate, blood pressure), urine output and clinical response.If you are well perfused and hydrated, but not producing adequate amounts of urine, medications can be given to help your kidney get rid of excess water in the body. These medications are usually reserved as second line treatments and should only be given once you have been well hydrated.If you have any medical conditions such as diabetes, you are at higher risk for certain procedures that involve any injection of dye or contrast, such as CAT scans and angiograms (a procedure involving injection of contrast into the blood vessels of the heart). If this is the case, you will be given fluids through the veins in your arms and medications such as N-acetylcysteine can be administered before the procedure to help minimize the insult to your kidneys. - Treat the precipitating cause.
Depending on the cause of your kidney failure, different steps can be taken to remove the precipitating factor for your episode of kidney failure.
If your kidney failure is due to loss of blood or other bodily fluids, resulting in dehydration, you should be rehydrated with abundant fluids (as described above). If you are experiencing an infection in the body, a range of blood tests, imaging (chest x-ray, abdominal X-ray or ultrasound), urine tests and other investigations should be performed to help determine the source of infection. Once this has been determined, antibiotics that don’t have effects on the kidney can be given to help treat the infection.A post renal cause of kidney failure such as an obstruction to the kidneys or urinary system should be promptly dealt with. - Treat the complications
The most important complications of ARF that require correction include:- Elevated blood potassium levels – this is a serious condition that should be treated as soon as it arises. If you have high levels of potassium in the body, a range of muscles in the body(especially the heart muscle) can fail to function properly and there is an increased risk of abnormal heart rhythms, dysfunction/paralysis of muscles and fits.
Doctors can help lower the body’s potassium levels by giving you calcium supplements through the veins, and trying to increase the uptake of calcium into cells by methods such as salbutamol (Ventolin) nebulisers and /or insulin – dextrose infusions. Potassium can also be removed from the body by administering potassium binding medications or dialysis (as a last resort). In the longer term, you may have to watch the potassium intake in your diet and avoid foods high in potassium such as bananas, nuts, and bran. - There can also be abnormal levels of other electrolytes and ions in the body, which the kidney helps to control, such as phosphate and calcium. In cases of kidney failure, these electrolytes aren’t excreted properly and modification of the diet should occur, with restriction of foods high in these electrolytes. Fluid restriction is also important in the management of kidney failure, to prevent accumulation of excess fluid not cleared by the kidneys.
- Pulmonary oedema (accumulation of fluid in the lungs) – If you experience excessive accumulation of fluid in the body, some fluid can enter the lungs and interfere with your normal breathing processes. Oxygen can be given to help you breathe and close monitoring of your vital signs should be performed. Medications such as diuretics (different classes act on different parts of the kidney) can be given to help decrease the amount of fluid in the body. Morphine may also be given to decrease any pain and anxiety that you experience. If there is no response to any of the above measures, specialist advice is sought and you may need to be started on dialysis.
- Increased tendencies to bleed – the kidneys are involved in producing hormones that help regulate the concentrations of red blood cells in the body and platelet function. When the kidneys dysfunction, there may be low levels of red blood cells and increased tendencies to bleeding. This may require the administration of blood transfusions, specific hormones that the kidneys produce, or platelets.
- Infection – If you experience any symptoms of infection, (eg fever, rash, chills/rigors), a clinical workup and /or antibiotics may be administered.
The outcome of patients with kidney failure is largely dependent on the cause of the acute deterioration and the provision of both supportive and medical treatments. Dialysis is a treatment that is reserved for patients who are not responsive or deteriorating despite the treatments described above, to allow the body to function in the setting of severe kidney failure.
- Elevated blood potassium levels – this is a serious condition that should be treated as soon as it arises. If you have high levels of potassium in the body, a range of muscles in the body(especially the heart muscle) can fail to function properly and there is an increased risk of abnormal heart rhythms, dysfunction/paralysis of muscles and fits.
- General Measures
Renal Failure – Acute References
-
-
- Agraharkar M. Acute Renal Failure, E-medicine [serial online]. 2007 [cited 14th August 2007]. Available from URL: http://www.emedicine.com/med/topic1595.htm
- Atkins R, Post-streptococcal glomerulonephritis in Indigenous communities in Australia, MJA 2001; 174: 489-490.
- Bhandari S, Turney J, Survivors of acute renal failure who do not recover renal function, QJM, 1996; 489 :415-421.
- Briganti E, McNeil J, Atkins R, The epidemiology of diseases of the kidney and urinary tract: an Australian perspective [online] 1999 [cited 13th August 2007]. Available from URL: www.med.monash.edu.au/Epidemiology/general_info/publications.html
- Brivet F, Kleinknecht D, Loirat P, et al. Acute renal failure in intensive care units: causes, outcome, and prognostic factors of hospital mortality: a prospective, multicenter study, Crit Care Med, 1996; 24:192-198.
- Kidney Health Australia, Nephritis – Glomerulonephritis [online] 2005 [cited 13th August 2007]. Available from URL: http://www.kidney.org.au
- Lameire N, Biesen W, Vanholder R. Acute renal failure, The Lancet, 2005; 365(9457): 417-430.
- Longmore JM, Hope RA, Longmore M. et al. Oxford Handbook of Specialties; USA: Oxford University Press Inc. 2001.
- Thomas M. Lecture notes – Acute Renal Failure – A Bedside Approach, Renal Consultant and UWA Lecturer, Royal Perth Hospital, 2007.
- Thomas M. Powerpoint presentation – Acute Renal Failure, Renal Consultant and UWA Lecturer, Royal Perth Hospital, 2007.
- Uchino S, Kellum J, Bellomo R, et al; for the Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators, Acute Renal Failure in Critically Ill Patients: A Multinational, Multicenter Study, JAMA 2005; 294:813-818.
- Venkataraman R, Prevention of acute renal failure, Chest, 2007; 131(1): 300-308.
-
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







