- What is Rectal Cancer (Adenocarcinoma of the Rectum)
- Statistics on Rectal Cancer (Adenocarcinoma of the Rectum)
- Risk Factors for Rectal Cancer (Adenocarcinoma of the Rectum)
- Progression of Rectal Cancer (Adenocarcinoma of the Rectum)
- Symptoms of Rectal Cancer (Adenocarcinoma of the Rectum)
- Clinical Examination of Rectal Cancer (Adenocarcinoma of the Rectum)
- How is Rectal Cancer (Adenocarcinoma of the Rectum) Diagnosed?
- Prognosis of Rectal Cancer (Adenocarcinoma of the Rectum)
- How is Rectal Cancer (Adenocarcinoma of the Rectum) Treated?
What is Rectal Cancer (Adenocarcinoma of the Rectum)
Rectal cancer may be of the adenocarcinoma type and usually arise from the epithelium (the layer of cells) which lines the large intestine.
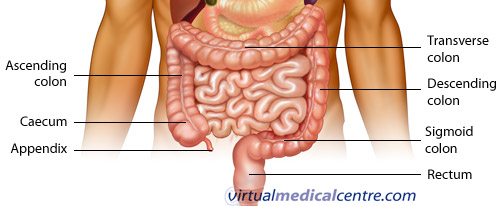
The colon is part of the large bowel. The large bowel starts at the end of the small bowel (the ileum), at the caecum. The caecum has the appendix running off it. The start of the colon is the ascending colon and where this rises to meet the liver (the hepatic flexure) it becomes the transverse colon. The transverse colon goes across the upper abdomen until it becomes adjacent to the spleen (the splenic flexure) and at this point it becomes the descending colon. The large bowel at this point goes down the abdomen to the pelvis at which point it becomes the sigmoid colon (because it curves in an “S” shape, sigma being the Greek for “S”). The sigmoid colon terminates at the rectum, which acts as a storage pouch for faeces before it is evacuated through the anus.
Overall, the function of the large bowel is to absorb water from stools. When the ilium enters its contents into the caecum, they are extremely liquid and gradually solidify as the contents progress around the large bowel.
Statistics on Rectal Cancer (Adenocarcinoma of the Rectum)
Rectal cancer is common but occurs very rarely in young adults. Rectal cancer becomes more common as age increases. People in their 50s, 60s and 70s are most at risk with with sex incidence being slightly more common in females.
Geographically, the rectal cancer tumour is found worldwide, but rectal cancer si most common in areas which have low fibre diets. Areas of the world with high fat consumption and low fibre consumption such as Europe, USA and Australia.
Risk Factors for Rectal Cancer (Adenocarcinoma of the Rectum)
There are a number of factors which increase the risk of developing rectal cancer:
- Hereditary conditions: At particularly high risk of Rectal cancer are people with hereditary conditions such as Familial Adenomatous Polyposis or Hereditary Non Polyposis Colorectal Cancer. In these conditions, it can occur even in young adults, e.g. late teens and early 20s.
- Family history of rectal cancer: First degree relatives of patients with rectal cancer have an increased risk, particularly if the relative develops rectal cancer at a young age.
- Polyps: Certain types of polyps, notably villous adenomas have a potential to become malignant. Rectal cancer patients who have previously had a polyp in the large bowel should undergo regular colonoscopy (ask your doctor how often).
- Inflammatory bowel disease: Patients who suffer from ulcerative colitis, have approximately a ten fold risk of developing the disease and should have a colonoscopy carried out regularly.
- Diet: A high fat, low fibre diet, especially if high in red meat, is the worst diet that predisposes people to rectal cancer. People who suffer from obesity are also at an increased risk.
Progression of Rectal Cancer (Adenocarcinoma of the Rectum)
The rectal cancer tumour spreads by invading the bowel wall. Once it crosses through the muscle layer within the bowel wall, it enters the lymphatic vessels, spreading to local and then regional lymph nodes. Sometimes rectal cancer spread via the blood stream to the liver, which is the most common area of metastasis from this tumour. Other organs that may be affected by blood borne spread are the lungs, less often the bones, and even less often the brain.
If a lot of tumour cells get through the bowel wall, they tend to float around as a small amount of fluid within the abdomen and can seed the covering of the bowel (peritoneum). This type of seeding produces small nodules throughout the abdomen which irritates tissues and causes the production of large amounts of ascites (fluid). Direct spread from the rectum may attach the tumour to the bladder in males and cause fistulas. In females it may invade the vagina or adjacent pelvic organs.
How is Rectal Cancer (Adenocarcinoma of the Rectum) Diagnosed?
General investigations into rectal cancermay show anaemia or an abnormal liver function test. The blood albumin level may be low (Albumin is produced mainly in the liver. It helps to keep the blood from leaking out of blood vessels. When albumin levels drop, fluid may collect in the ankles, lungs, or abdomen). If liver involvement is severe the clotting profile will be abnormal with a raised INR.
Prognosis of Rectal Cancer (Adenocarcinoma of the Rectum)
Early rectal cancers have extremely good prognosis. If they have not invaded through the muscle wall, the vast majority of them are cured by surgery. Once the tumour has breached the muscular wall and gone to the regional lymph nodes, over 60% of rectal cancer patients will still survive at least 5 years. If the rectal cancer tumour has spread to other organs such as the liver or lung, the current 5 year survival is approximately 10%.
5 year survival by stage is:
- Dukes A: 90% 5 YS
- Dukes B: 70% 5 YS
- Dukes C: 50% 5 YS
- Dukes D: 10% 5 YS
There have also been attempts to further classify each stage further, especially Dukes B and C using TNM style classification. This gives Stages I to IV (being approximately equivalent to the Dukes Stages, but giving Stage IIA and B, Stage IIIA snd B etc. The prognosis of IIIA approaches that of IIB etc. This is not yet in widespread use).
The advent of the newer chemotherapy agents has made a significant impact on rectal cancer prognosis. Irinotecan and oxaliplatin combined with 5FU offer significant benefits over the long time gold standard of 5 day bolus dose 5FU – the Mayo regime. Newer agents, notably the biological agents bevacizumab and cetuximab look like they will significantly increase the prognosis of these rectal cancer tumours.
How is Rectal Cancer (Adenocarcinoma of the Rectum) Treated?
The rectal cancer treatment of choice is clearly surgery for early disease. For Dukes Stage A tumours (that have not reached the muscular layer within the bowel wall) this will usually be curative in approximately 90% of cases.
Rectal cancer surgery involves usually 1 of 2 methods:
- Anterior Resection is where the rectum is resected from an operation from the front. The Anus is retained, along with anal function.
- Abdomino-Peroneal Resection is usually carried out for tumours low down in the rectum and requires the removal of the Anus. A colostomy is then necessary.
Sometimes, a colostomy may be used in a temporary way for any bowel surgery, as a protective method to allow the intended surgery to heal. Rectal cancer surgery is usually carried out to remove the primary tumour for all except Dukes D (Stage IV disease. In some cases of Dukes D disease, if the bowel looks as though it will become obstructed, the primary tumour may be resected.
If the rectal cancer has breached the bowel wall, and especially if it is has gone into the local lymph nodes, adjuvant chemotherapy will increase the chance of cure. The same is true if it has spread to regional lymph nodes. There is a clear consensus of opinion that Dukes Stage C should receive adjuvant chemotherapy. Dukes B tumours may also benefit from adjuvant treatment. This decision is made on an individual basis.
If the rectal cancer has spread further, such as to the liver, longer term palliation can still be achieved by surgery to the primary tumour to prevent bowel obstruction, followed by specific treatment for the metastases.
Chemotherapy regimes
Standard adjuvant therapy is 5-fluorouracil and calcium folinate given for six months. Standard therapy for metastatic disease is irinotecan, 5-fluorouracil and leucovorin. Each of the agents in this regime is administered by IV injection weekly for 4 weeks every 6 weeks. For liver metastases, a new technique is to place radioactive material into the blood vessels that supply the liver. The radioactive material impacts in the blood vessels supplying the tumour and irradiates tumour from within. This can be combined with chemotherapy in an attempt to mop up any other tumour cells which have spread elsewhere. Watch this site for further rectal cancer news.
If there is just a solitary liver metastases in one side of the liver, there is quite a strong argument for surgery to remove the single metastases in rectal cancer patients who are physically otherwise quite well. Following liver resection, chemotherapy would normally be given.
If the rectal cancer has spread to bone and is causing pain, local radiotherapy can be very useful at controlling local symptoms. Because of the anatomical situation of the rectum, (relatively away from the other parts of the bowel) radiotherapy is often given after surgery as adjuvant treatment. For recurrent local disease, radiotherapy also has a really important part in stopping it from spreading.
Improvement in rectal cancer symptoms is an important measurement. Specific monitoring may be by measurement of serum CEA. If curative surgical resection has been achieved, repeated checks on a yearly basis by colonoscopy are advisable. Imaging is normally carried out either by ultrasound or CT to check for recurrence in the liver or lymph nodes. For metastatic disease, serum CEA can be very helpful in gauging response to treatment. Abnormal liver function tests can be monitored and imaging of any soft tissue metastases such as in the liver or lung can be performed.
The rectal cancer symptoms that may require attention are fatigue from anaemia and the feeling of tenesmus (wanting to open the bowels when there is no stool there can be particularly distressing, especially when it is painful). Rectal cancer patients may require treatment for visceral pain from liver metastases and less commonly for somatic pain from bone metastases. If lung metastases are present there may be pleural effusions causing breathlessness. Effusions may require drainage.
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







