- What is emergency contraception?
- Methods of emergency contraception
- When is emergency contraception used?
- Who can use emergency contraception?
- How popular is emergency contraception?
- How does emergency contraception work?
- How effective is emergency contraception?
- How safe are emergency contraception methods?
- Where can you get emergency contraceptives?
- How do you use emergency contraceptives?
- Contraindications of emergency contraception
- Side effects and complications of emergency contraception
- Important points about emergency contraception
What is emergency contraception?

Methods of emergency contraception
There are a number of emergency conctraceptive methods:
- Hormonal emergency contraceptives, commonly referred to as ‘the morning after pill’;
- Intrauterine contraceptive devices (IUDs), which are also used for long-term contraception;
- Mifepristone, also known as RU486. This medicine is most commonly used to induce first (and less commonly second) trimester abortion.
In Australia, only hormonal emergency contraceptives and IUDs are available for emergency contraception.
Hormonal emergency contraceptive pills (morning after pill)
The emergency contraceptive pill, also known as the morning after pill, contains the female hormones oestrogen and progestogen. It is similar to the oral contraceptive pill, but the doses of hormones are very different. The morning after pill may either have both oestrogen and progestogen, or progestogen only.
The first methods of emergency contraception were introduced in the 1960s and consisted of high doses of oestrogen. This is rarely used today because of the frequently experienced side effects of severe nausea and vomiting. Later, the Yuzpe regime (named after the Canadian doctor who developed it) became widely popular. The Yuzpe method used a combination of ethinyl oestradiol (an oestrogen) and levonorgestrel (a progestogen). Again, side effects were experienced by over half of all women.
It was soon found that progestogen alone was more effective and had fewer side effects, and was eventually approved for use as an emergency contraceptive. The progestogen-only regime prevents 85% of expected pregnancies, compared to the 76% prevented by the Yupze method, and is the recommended method of hormonal emergency contraception today, although the Yuzpe combination pill is still available.
In Australia, there are two types of morning after pills available:
- Progestogen-only pills (e.g. Postinor-2, Levonelle-2, NorLevo) have been available in Australia since 2002. They come as two single tablets, each containing levonorgestrel.
- The older combination pill (e.g. Microgynon 30, Levlen Ed, Nordette, Monofeme) contains two hormones and comes in a pack of four pills. All four pills are taken as soon as possible following unprotected sex, within 4–12 hours. Combination pills are only recommended if the other option is not available.
Intrauterine devices
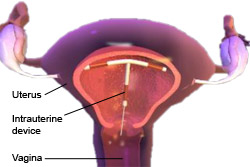 |
|
Image courtesy of Blausen Medical Communications. |
The copper intrauterine device (IUD) can be employed as an emergency contraceptive. This device is fitted inside the uterus, and is normally use as a long term contraceptive method.
The copper IUD can provide effective emergency contraception up to five days after unprotected sex, and is most often used when a woman presents more than 72 hours after intercourse. If intercourse has taken place before ovulation, the IUD can be inserted five days after sexual intercourse. It is substantially more effective than hormonal methods and can reduce the risk of pregnancy by 99%.
The copper IUD is usually not recommended for women who are exposed to or are at high risk of having a sexually transmitted infection (STI).It may not be suitable for younger women who have never given birth. Another drawback is the complex and invasive insertion process, which requires a skilled practicioner. Nevertheless, it is highly effective, and can be inserted during any time of the menstrual cycle.
The hormonal or levonorgestrel intrauterine system is currently not available to be used as an EC.
 |
For more information, see Intrauterine Device. |
Mifepristone is a medicine developed in France in 1980. It is mainly used to induce first and second trimester abortion, but it can also be used as an emergency contraceptive. It is a highly effective EC, although the availability of the drug is severely restricted in Australia and it is not available for use as an EC. Thus far, it is only licensed for use as an EC in China.
When is emergency contraception used?
Emergency contraception is designed to prevent pregnancy following sexual intercourse in situations where:
- No contraceptive method was used;
- A contraceptive method has failed (e.g. a condom breaks, or a woman forgets to take the oral contraceptive pill for two or more consecutive days and sexual intercourse occurs); or
- Sexual assault occurs.
Emergency contraceptives are most effective the sooner they are used after unprotected sex. Morning after pills are very effective if used within 24 hours, and are reasonably effective if taken up to five days after intercourse. IUDs are effective up to seven days after intercourse.
Who can use emergency contraception?
Any woman is able to take the morning after pill, even if they are unable to take oral contraceptive pills because of other health issues (e.g. migraine or thrombosis).This is because of the short exposure time to the hormones within the morning after pill.
The use of copper IUDs as an emergency contraceptive is more restricted. It is not ideal for certain women, particularly women who have never given birth, women with STIs, or women at high risk of contracting STIs.
How popular is emergency contraception?
Evidence suggests that increasing the availability of emergency contraceptives does not increase risk-taking behaviours, and does reduce unwanted pregnancies. Studies have shown that educating teenagers about emergency contraception does not influence sexual activity.
How does emergency contraception work?
Different ECs work in different ways to prevent pregnancy.
Hormonal ECs
Hormonal ECs prevent pregnancy by inhibiting ovulation. When ovulation is prevented, an egg is not released from the woman’s ovaries and cannot be fertilised. It is important to note that ECs can only be used effectively before ovulation occurs (at about the middle of the menstrual cycle).
IUDs
IUDs prevent pregnancy by inhibiting the implantation of an embryo in the woman’s womb. An embryo is a fertilised egg. If a fertilised egg implants in the woman’s womb, it will form a pregnancy. If implantation does not occur, the embryo cannot grow and the woman does not become pregnant. When an IUD is inserted, it changes the appearance and chemistry of the womb, and these changes prevent implantation of an embryo.
Mifepristone
Mifepristone also prevents pregnancy by affecting the receptivity of the woman’s womb to a fertilised egg. It does this by blocking the action of progesterone, a hormone which is needed to ensure a fertilised egg implants in the womb and remains attached to the wall of the womb.
How effective is emergency contraception?
The risk of pregnancy occurring is about 2 per 100 women taking the morning after pill following unprotected sex. The morning after pill is most effective if it is taken within 12 hours after unprotected sex.If taken within 1 day of unprotected sex, the progestogen-only pills are effective in about 85–90% of cases. If it is taken 3–5 days afterwards, the effectiveness is reduced to about 60%.The combined oestrogen–progestogen morning after pill is at least 75% effective if taken within 3 days of unprotected sex.
The morning after pill will probably not work if:
- More than three days has passed since the episode of unprotected sex;
- Vomiting occurs after taking the pill; and
- Another episode of unprotected sex occurs before the next period.
Copper IUDs are 97–99% effective when they are inserted within 5 days of sexual intercourse.
How safe are emergency contraceptive methods?
Hormonal emergency contraception is safe for almost all women to use, including women who are advised against using oral contraceptives. The morning after pill has a very short exposure time and a low total hormone concentration.
The copper IUD is considered to be a safe contraceptive method, although it is associated with higher risks of complications such as pelvic inflammatory disease and irregular bleeding.
Where can you get emergency contraceptives?
In Australia, the morning after pill is available over the counter from pharmacies. It is also available from hospital emergency departments or sexual health clinics. It is available without a prescription in a range of countries, including Canada, India, Sweden, UK and France.In the US, morning after pills became available over the counter in 2006 for women aged over 18 years.
Copper IUDs must be obtained from a general practitioner and fitted by a trained professional.
How do you use emergency contraceptives?

The morning after pill is available as either one 1.5 mg tablet or two 0.75 mg tablets. The first tablet should be taken within 72 hours of intercourse, and the second pill 12 hours after the first.
If vomiting occurs within two hours of taking the morning after pill, it must be taken again.
Contraindications of emergency contraception
The only contraindication for the use of hormonal emergency contraception is a confirmed pregnancy, primarily because the morning after pill will have no effect at this stage. If the morning after pill is taken during pregnancy, it will have no impact on the pregnancy and will not harm the foetus.
Due to the risk of irregular vaginal bleeding and spotting associated with IUDs, women taking anticoagulants should not use an IUD.
Emergency contraception should not be used repeatedly as a contraceptive program. Long term contraceptive methods (e.g. condoms, the pill) are more effective.
Side effects and complications of emergency contraception
Nausea and vomiting are the most frequent side effects experienced with hormonal emergency contraception pills. This occurs in about 5% of women using the progestogen-only morning after pill, and in nearly 20% of women using the combined pill. If vomiting occurs within two hours of taking the pill, the dosage must be taken again.
Other potential side effects include:
- Dizziness
- Tiredness
- Headache
- Breast tenderness
- Spot bleeding
- Lower abdominal pain
These side effects occur more frequently with the combined pill compared to the levonorgestrel pill, and usually subside after 48 hours.
About 30% of women experience a delay in their next period, usually of a week. If a period does not come within four weeks of taking the pill, a pregnancy test is advised.
Oral contraceptives are associated with an increased risk of venous disease (e.g. deep vein thrombosis) due to third generation progestogens. It is thought that morning after pills may have a similar effect, though the shorter exposure time makes it unlikely. Studies have not yet been conclusive.
Side effects associated with IUDs include irregular vaginal bleeding, spotting and cramping. Other potential complications with IUDs included an increased risk of pelvic inflammatory disease and subsequent infertility if untreated. IUDs may lead to reduced fertility in women who have never given birth.
Important points about emergency contraception

A common misconception is that morning after pills can only be taken the ‘morning after’ the act of unprotected sex, perhaps due to the casual term ‘morning after pill’. Despite it’s name, the morning after pill can be taken up to five days after intercourse, although it is best taken as soon as possible.
It should also be emphasised that:
- Emergency contraception cannot prevent STIs; and
- Emergency contraception does not cause abortion.
More information
 |
For more information on different types of contraception, male and female anatomy and related health issues, see Contraception. |
References
- Emergency contraception [online]. Brisbane, QLD: Queensland Health; 28 April 2008 [cited 20 October 2008]. Available from: URL link
- Bastianelli C, Farris M, Benagiano G. Emergency contraception: A review. Eur J Contracept Reprod Health Care. 2008;13(1):9-16. [Abstract]
- Trussell J, Rodríguez G, Ellertson C. New estimates of the effectiveness of the Yuzpe regimen of emergency contraception. Contraception. 1998;57(6):363-9. [Abstract]
- Foran T. Emergency contraception. Aust Fam Physician. 2002;31(10):909-12. [Abstract | Full text]
- Emergency contraception fact sheet [online]. Ashfield, NSW: Family Planning NSW. February 2008 [cited 28 October 2008]. Available from: URL link
- Glasier A. Emergency contraception. Best Pract Res Clin Obstet Gynaecol. 2002;16(2):181-91. [Abstract]
- Trussell J, Ellertson C, Stewart F, et al. The role of emergency contraception. Am J Obstet Gynecol. 2004;190(Suppl):S30-8. [Abstract]
- LaValleur J. Emergency contraception. Obstet Gynecol Clin North Am. 2000;27(4):817-39. [Abstract]
- Emergency contraception [online]. Woodville, SA: Sexual Health Information Networking and Education SA; 11 November 2008 [cited 20 October 2008]. Available from: URL link
- Brunton J, Beal MW. Current issues in emergency contraception: An overview for providers. J Midwifery Womens Health. 2006;51(6):457-63. [Abstract]
- Turner AN, Ellertson C. How safe is emergency contraception? Drug Saf. 2002;25(10):695-706. [Abstract]
- Family planning: A global handbook for providers [online]. Bethesda, MD: Knowledge for Health Project; 2007 [cited 25 January 2011]. Available from: URL link
- Trussel R, Raymand EG. Emergency contraception: A last chance to prevent unintended pregnancy [online]. 2010 [cited 25 January 2011]. Available from: URL link
- De Costa CM. Medical abortion for Australian women: It’s time. Med J Aust. 2005;183(7):378-80. [Abstract | Full text]
- Emergency contraception [online]. Fortitude Valley, QLD: Family Planning Queensland; August 2008 [cited 3 February 2011]. Available from: URL link
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







