- What is Invasive Breast Carcinoma (Breast Cancer)?
- Statistics
- Risk Factors
- Progression
- Symptoms
- Clinical Examination
- How is it Diagnosed
- Treatment
- References
What is Invasive Breast Carcinoma (Breast Cancer)?
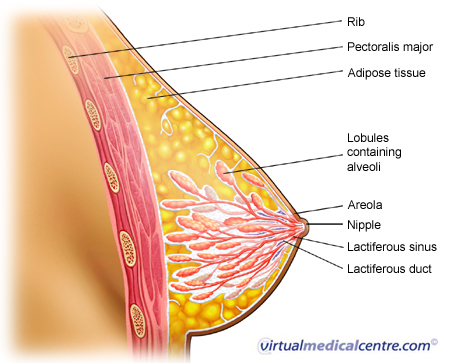
Invasive breast carcinomas are cancers originating from breast tissue. They may originate in the milk ducts and/or glandular (breast milk producing) tissue of the breast and invade into normal healthy tissues. There are several different types of breast cancer, but infiltrating ductal carcinoma is the most common type of invasive breast cancer accounting for 70 to 80% of invasive lesions.
The major types of invasive breast carcinomas are:
- Ductal carcinoma (70–80%)- Cancer cells that resemble the ducts of the breast;
- Lobular carcinoma (5–10%)- Cancer cells that resemble the lobules or glands of the breast;
- Medullary carcinoma (1–5%);
- Mucinous carcinoma (1–6%); and
- Tubular carcinoma (2%).
In situ carcinomas of the breast such as ductal carcinoma in situ (DCIS) and lobular carcinoma in situ (LCIS) refer to lesions confined to the breast ducts or lobules (do not invade into normal healthy tissues) and are discussed separately.
 |
For more information about breast cancer, including types, treatments, animations and more, see Breast Cancer. |
Statistics
In Australia in 2008 there were 13,680 invasive breast cancer diagnoses. 99% were made in women. Invasive breast cancer is classified according to the type of breast cells it affects. In 2008 the majority (78%) of invasive breast cancers were ductal (arising in the milk ducts and thought to be related to pre-invasive ductal carcinoma in situ). Of the remainder, 11% originated in the breast lobules (possibly related to pre-invasive lobular carcinoma in situ) and 5% arose in unspecified breast tissues.
Other types of invasive breast cancer include: tubular carcinoma and invasive cribriform carcinoma, medullary carcinoma and atypical medullary carcinoma, mucinous carcinoma, invasive papillary carcinoma and inflammatory carcinoma. Approximately 1% of all types of invasive carcinomas of the breast are male breast cancer.
Invasive breast cancer is diagnosed in 115 per 100,000 Australia women each year, compared to approximately 1 per 100,000 for men. This is an increase from 44 diagnoses per 100,000 people (men and women) in 1982, to 60 per 100,000 in 2011. 1 in 8 women will be diagnosed with breast cancer before their 85th birthday compared to 1 in 719 men. Breast cancer diagnoses per person in Australia are similar to those in New Zealand and western and northern European countries and higher than those in southern and eastern European countries.
The risk of invasive breast cancer increases with increasing age. The number of people diagnoses with breast cancer each year increases from less than 1 per 100,000 amongst people aged 20-24 years, to 62 per 100,000 amongst 40-44 year olds and 172 per 100,000 amongst 60-64 year olds. Amongst those aged over 85 years, 200 per 100,000 people are diagnosed with breast cancer each year, predominately women. The average age of breast cancer diagnosis is 60 years.
In 2012, invasive breast cancer caused 2,819 deaths. It was the second leading cause of cancer-related death amongst women (following lung cancer). Although the absolute number of people who died from breast cancer increase from 1,435 in 1968, the rate per person declined from 17 deaths per 100,000 people to 11 per 100,000 in the period. The proportion of people which survived for five years following a breast cancer diagnosis was 90% in the period 2007-2011 (compared to 67.5% for all cancers), up from 72% in 1982-1986. The average age of breast cancer death in females increased from 64 years in 1982 to 68 years in 2008. Average age of death in males with breast cancer ranged from 63 years in 1999 to 72 years in 2007.
Risk Factors
The risk factors for breast cancer are:
Increasing age- The risk of breast cancer increases with age. Most women diagnosed with breast cancer in Australia were in the 50–69 age group.
- Female gender- Breast cancer occurs more than 100 times more frequently in women than in men.
- Increased exposure to oestrogen produced by the body (endogenous oestrogen) – The factors that result in exposure to oestrogen include early menarche (onset of menstruation), nulliparity (women who have not borne a child before), late age at first full-term pregnancy and later menopause (cessation of menstruation).
- Family history and hereditary breast cancer syndromes- Women with a family history of breast cancer are at higher risk for breast cancer. Women with inherited gene abnormalities/mutations such as BRCA1 and BRCA2 mutations are also at higher risk.
- Lifestyle factors- Regular physical exercise has been found to be associated with lower risk of breast cancer. Conversely, cigarette smoking has been found to increase the risk of breast cancer.
- Benign breast diseases- Complex fibroadenoma (non-cancerous tumour of the breast), atypical hyperplasia (accumulation of abnormal cells in a breast duct), sclerosing adenosis (excessive growth of tissues in the breast lobules) and intraductal papillomas (non-cancerous tumour of the breast duct)
Symptoms
Breast symptoms
The presence of breast symptoms may suggest underlying breast cancer and requires further investigation and management. The most frequent symptoms of breast cancer are: breast lump, mastalgia (breast pain), nipple changes, breast asymmetry/skin dimpling and nipple discharge. Nipple changes which require urgent referral include recent inversion, change in shape or rash involving the nipple or areola (pigmented area around nipple).
Women presenting to a doctor with breast symptoms may be asked about the location of the symptom, its duration and the symptom’s relationship to woman’s menstrual cycle.
Symptoms due to spread of breast cancer
Breast cancer may spread to the lymph nodes, bones, liver and lungs. Enlarged axillary lymph nodes, respiratory symptoms such as recurrent lower respiratory tract infections, bone pain and jaundice due to liver metastasis may be indicators of breast cancer that has spread.
How is it Diagnosed
If breast cancer is suspected, your doctor may take a history and examine you. In addition, he/she might order imaging tests as well as obtain tissue biopsy (suspected abnormal tissue removed to be studied under the microscope). This combination of tests is otherwise known as the ‘triple test’ approach to diagnosis.
Imaging tests

Mammography is often the first line imaging modality used to reveal an underlying abnormality in the breast. Mammography is recommended as the first imaging test in people aged over 50.
Ultrasound
Ultrasound is another imaging method that is useful in the diagnosis of breast disease. It can be used to distinguish solid mass lesions from cysts (fluid containing masses). It also helps guide your health professional to obtain biopsies of suspicious looking breast tissue. Ultrasound is more often used in younger women, who have denser breast tissue. Ultrasound is recommended as the first imaging modality in people under 35 years of age. Mammography and targeted ultrasound can be used in conjunction for the evaluation of symptomatic women between 35 and 50 years of age.
Magnetic resonance imaging (MRI)
Breast MRI is useful for diagnosing breast cancer which does not show up on mammography.
Tissue biopsy
The two methods of obtaining tissue samples for microscopic examination are fine needle aspiration and core biopsy. Both techniques are often used in conjunction as they are complementary. Fine needle aspiration biopsy involves passing a needle attached to a syringe back and forth within the lesion so as to obtain sufficient cells to be studied by the pathologist. Core biopsy involves passing a larger width needle through the skin to take a sample of tissue from the breast.
Core biopsy can sometimes demonstrate invasive disease whereas fine needle aspiration would not be able to distinguish between in situ (cancer which has not spread to normal healthy tissue) and invasive cancer.
Treatment
The management of invasive breast carcinoma is dependent on the stage of the cancer. Once the diagnosis of cancer has been made, the disease should be staged to determine how much the tumour has spread. Staging of cancers involves clinical evaluation, blood tests (full blood count, liver function tests) and imaging tests including chest x-rays, abdominal ultrasound/CT and isotope bone scans to look for distant metastasis. Treatment would also be dependent on variables such as the microscopic appearance and hormonal receptor status (whether the tumour has certain genetic markers) of the tumour. In general, treatment of invasive breast carcinoma involves a combination of medical, surgical and radiation therapy.
Medical therapy
Medical therapy may be divided further into hormonal therapy, chemotherapy and biological therapy. The aims of medical therapy may be neoadjuvant (aims to reduce tumour size before surgery), adjuvant (aims to cure the cancer) or palliative (aims to relieve symptoms but is not curative). Neoadjuvant systemic therapy is given prior to surgery or radiation therapy in order to improve outcomes. It may increase the chance of preserving more normal breast tissue and enable removal of locally advanced cancers.
Adjuvant systemic therapy is administered after surgery to prevent breast cancer recurrence and improve overall survival with a curative intent. Palliative systemic therapy is administered in patients with non-operable or advanced breast carcinoma with the aim of optimising quality of life and relieving symptoms due to the disease.
Hormonal therapy
The goal of hormonal or endocrine therapy is to prevent breast cancer cells from being stimulated by the oestrogen naturally produced by the body. It is most often used in women with breast tumours expressing oestrogen or progesterone receptors which is determined by the pathology lab. This prevention of stimulation by oestrogen can be achieved with pharmacological agents:
- Selective oestrogen receptor modulators (e.g. tamoxifen) block oestrogen receptors;
- Luteinising hormone-releasing hormone agonists (e.g. goserelin) prevent oestrogen synthesis by the ovaries;
- Aromatase inhibitors (e.g. letrozole) which suppress oestrogen levels in post-menopausal women by inhibiting aromatase which is required for synthesising oestrogens.
Biological agents
People who have breast carcinoma which produces Human Epidermal Growth Factor Receptor 2 (HER2) protein may benefit from biological agents such as trastuzumab. Trastuzumab is an artificially produced antibody that binds to the HER2 protein on breast cancer cell surfaces thus preventing further growth of the cancer.
Chemotherapy

Surgical therapy
The aim of surgical treatment is to control the disease within the breast and underlying chest wall. Complete removal of the breast (mastectomy) was previously the standard operation for invasive breast cancer but breast conservation surgery has become more prevalent in recent times. Surgical treatment may also involve axillary lymph node sampling or surgical clearance of axillary lymph nodes. Breast conservation surgery involves removing the tumour with a margin of surrounding breast tissue followed by radiotherapy to the breast to reduce local recurrence (regrowth of the tumour in the same location).
Radiation therapy
Radiation therapy is used after breast conservation surgery and mastectomy to reduce the risks of local recurrence. It involves the use of ionising radiation that damages the DNA of cancer tissue hence leading to cancer cell death.
References
- Australian Institute of Health and Welfare and Australasian Association of Cancer Registries 2010. Cancer in Australia: an overview, 2010. Cancer series no. 60. Cat. no. CAN 56. Canberra: AIHW [ Full Text]
- Australian Institute of Health and Welfare & National Breast and Ovarian Cancer Centre 2009. Breast Cancer in Australia: an overview, 2009. Cancer series no. 50. Cat. no. CAN 46. Canberra: AIHW. [Full Text]
- Australian Institute of Health and Welfare 2010. ACIM (Australian Cancer Incidence and Mortality) Books. AIHW: Canberra. [Book]
- Peto J, Mack TM. High constant incidence in twins and other relatives of women with breast cancer. Nat Genet. 2000; 26: 411. [Abstract]
- Burkitt HG, Quick CRG, Reed JB. Essential Surgery: problems, diagnosis and management. Philadelphia: Churchill Livingstone Elsevier; 2007. [Book]
- Kelsey JL, Gammon MD, John EM. Reproductive factors and breast cancer. Epidemiol Rev. 1993; 15: 36-47. [Abstract]
- Maruti SS, Willett WC, Feskanich D et al. A prospective study of age-specific physical activity and premenopausal breast cancer. J Natl Cancer Inst. 2008; 100: 728. [Abstract | Full Text]
- Band PR, Le ND, Fang R, et al. Carcinogenic and endocrine disrupting effects of cigarette smoke and risk of breast cancer. Lancet. 2002; 260: 1044. [Abstract]
- Li CI, Uribe DJ, Daling JR. Clinical characteristics of different histologic types of breast cancer. Br J Cancer. 2005; 93: 1046. [Abstract | Full Text]
- National Breast Cancer Centre. The investigation of a new breast symptom. Journal [serial on the Internet]. 2006 Date 2011 Mar 15]: Available from: [URL link]
- Disibio G, French SW. Metastatic patterns of cancers: results from a large autopsy study. Arch Pathol Lab Med. 2008; 132: 931-9. [Abstract | Full Text]
- Morrogh M, Morris EA, Liverman L et al. The predictive value of ductography and magnetic resonance imaging in the management of nipple discharge. Ann Surg Oncol. 2007; 14: 3369. [Abstract]
- Gralow JR, Burstein HJ, Wood W, et al. Preoperative therapy in invasive breast cancer: pathologic assessment and systemic issues in operable disease. J Clin Oncol. 2008; 26: 814. [Abstract]
- Early Breast Cancer Triallists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005; 365: 1687. [Abstract]
- Osborne CK, Yochmowitz MG, Knight WA, et al. The value of oestrogen and progesterone receptors in the treatment of breast cancer. Cancer. 1980; 46: 2884. [Abstract]
- Lucy, Armstrong, Goldman, et al; Drug Information Handbook; 16th ed. [Book]
- Shepard HM, Lewis GD, Sarup JC, et al. Monoclonal antibody therapy of human cancer: taking the HER2 protooncogene to the clinic. J Clin Immunol. 1991; 11: 117. [Abstract]
- Longmore M, Wilkinson IB, Turmezei T et al. Oxford handbook of clinical medicine. 7th ed. Oxford: Oxford University Press; 2007. [Book]
- Robbins SL, Cotran RS. Pathologic basis of disease. 7th edition. Elsevier Saunders, 2007. [URL Link]
- Australian Institute of Health and Welfare. Breast Cancer in Australia: an Overview 2012. Cancer series No. 71. Cat. No. CAN67. 2012. [cited 28 September 2015]. Available from: [URL Link]
- Cancer Australia. Breast Cancer in Australia. 2015. [cited 28 September 2015]. Available from: [URL Link]
- Australian Institute of Health and Welfare. Cancer in Australia: an Overview 2014. Cancer Series No. 90. Cat No. CAN88. [cited 28 September 2015]. Available from: [URL Link]
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.

 Increasing age- The risk of breast cancer increases with age. Most women diagnosed with breast cancer in Australia were in the 50–69 age group.
Increasing age- The risk of breast cancer increases with age. Most women diagnosed with breast cancer in Australia were in the 50–69 age group.





