RATIONALE: Drugs used in chemotherapy use different ways to stop tumor cells from dividing so they stop growing or die. Radiation therapy uses high-energy x-rays to damage tumor cells. Combining radiation therapy with chemotherapy may kill more tumor cells.
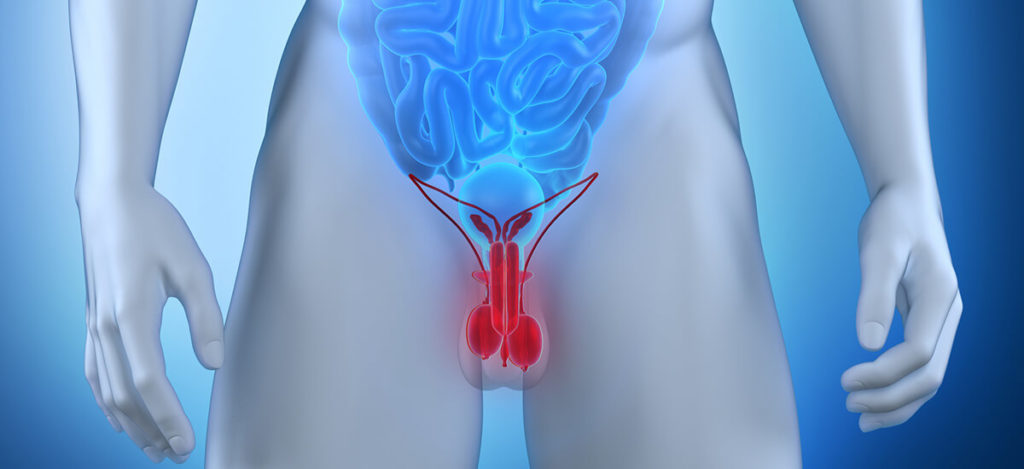
RATIONALE: Drugs used in chemotherapy use different ways to stop tumor cells from dividing so they stop growing or die. Radiation therapy uses high-energy x-rays to damage tumor cells. Combining radiation therapy with chemotherapy may kill more tumor cells. PURPOSE: Phase I/II trial to study the effectiveness of chemotherapy and radiation therapy in treating infants who have tumors of the brain. Condition:- childhood brain tumor- Neuroblastoma Study Type: InterventionalStudy Design: Treatment Official Title: Phase I/II Pilot Study of Systemic and Intrathecal Chemotherapy Followed By Conformal Radiotherapy in Infants With Embryonal Intracranial Central Nervous System Tumors Further Study Details: OBJECTIVES:Assess the feasibility of the addition of regional therapy with intrathecal (IT) mafosfamide to an intensive regimen of systemic chemotherapy in children under 3 years of age at diagnosis with medulloblastoma/primitive neuroectodermal tumor, ependymoma with metastatic disease, or other primary intracranial embryonal tumors. Determine the safety and feasibility of a limited dose- escalation schedule of IT mafosfamide in this patient population. Assess the feasibility, including expected disease progression, of delivering 20 weeks of systemic chemotherapy plus IT mafosfamide in this patient population. Determine the subsequent progression-free survival and pattern of failure associated with the use of IT mafosfamide and conformal irradiation to the local tumor region followed by 2 further courses of systemic chemotherapy among these patients with initially local disease (M0) at diagnosis. Develop preliminary estimates of the local and neuraxis response rate to intensive postoperative systemic/regional chemotherapy in these patients. Determine the acute and chronic toxic effects associated with the delivery of the first 20 weeks of this chemotherapy in these patients. Determine whether the first 10 weeks of systemic chemotherapy can restore normal CSF flow, thus permitting administration of IT mafosfamide during the second 10 weeks of systemic chemotherapy in patients initially ineligible to receive IT mafosfamide because of subarachnoid block by tumor. Assess the pharmacokinetics of IT mafosfamide using a limited sampling strategy in these patients. Determine the concentration of matrix metalloproteinases (MMPs) in the CSF of these patients. OUTLINE: This is a multicenter, dose-escalation study of mafosfamide. All patients receive regimen 1 chemotherapy. Children whose tumor is limited to 1 area at the beginning of the study proceed to radiotherapy and then regimen 2 chemotherapy. Children whose tumor is found in more than 1 part of the brain or in the CSF at the beginning of the study complete treatment after regimen 1 chemotherapy. Children with normal CSF flow at the beginning of the study receive regimen 1 chemotherapy along with intrathecal (IT) mafosfamide. Children with abnormal CSF flow receive regimen 1 without IT mafosfamide. Patients with initially abnormal CSF flow who show no evidence of obstructive hydrocephalus or compartmentalization on the repeat study receive IT mafosfamide beginning with course 2. Patients receive cyclophosphamide IV over 30 minutes twice weekly on weeks 1, 4, 11, and 14, vincristine IV once weekly on weeks 1-6 and 11-16, cisplatin IV over 6 hours once weekly on weeks 1, 4, 11, and 14, and oral etoposide once weekly on weeks 7-9 and 17-19. IT mafosfamide is administered twice weekly on weeks 1-6 and then once weekly on weeks 7-9, 11, 14, and 17. Patients are evaluated at weeks 10 and 20. After completion of regimen 1, patients may undergo surgery to remove more of their tumor. Patients who are initially M0 with stable or responding disease begin conformal radiotherapy 2 weeks after completing regimen 1 chemotherapy or second surgery. Patients receive radiotherapy once daily 5 days a week. Regimen 2: After completing radiotherapy, patients receive cyclophosphamide IV over 30 minutes twice weekly on weeks 1, 4, 11, and 14, vincristine IV once weekly on weeks 1-6 and 11-16, and oral etoposide once weekly on weeks 7-9 and 17-19. Patients are evaluated at weeks 10 and 20. Cohorts of 3-6 patients receive escalating doses of IT mafosfamide during regimen 1 chemotherapy until the maximum tolerated dose (MTD) is determined. The MTD is defined as the dose preceding that at which 2 of 3 or 2 of 6 patients experience dose-limiting toxicity. Patients are followed every 3 months for 1 year, every 4 months for 1 year, every 6 months for 2 years, and then annually thereafter. PROJECTED ACCRUAL: A total of 86-95 patients will be accrued for this study within 4-5 years. Eligibility Ages Eligible for Study: up to 2 Years, Genders Eligible for Study: Both Criteria DISEASE CHARACTERISTICS:Histologically confirmed primary intracranial CNS medulloblastoma/primitive neuroectodermal tumor or other embryonal tumor (medulloepithelioma, ependymoblastoma, neuroblastoma, pineoblastoma), atypical teratoid/rhabdoid tumor, intracranial germ cell tumor, choroid plexus tumor, or metastatic ependymoma If positive bone scan, pre-treatment bone marrow aspirate and biopsy must be free of tumor PATIENT CHARACTERISTICS: Age:Under 3 Performance status:Karnofsky 30-100% OR Lansky 30-100% Life expectancy:Not specified Hematopoietic:Hemoglobin at least 10 g/dL Absolute neutrophil count at least 1,500/mm^3 Platelet count at least 100,000/mm^3 Hepatic:Bilirubin less than 1.5 mg/dL SGPT less than 5 times upper limit of normal Renal:Creatinine normal OR Creatinine clearance greater than 40 mL/min Other:Willing to have a central line Willing to have CSF flow study to determine whether or not they will receive intrathecal chemotherapy Willing to have Ommaya reservoir placed if needed PRIOR CONCURRENT THERAPY: Biologic therapy:Not specified Chemotherapy:No prior chemotherapy Endocrine therapy:Prior steroids allowed Radiotherapy:No prior radiotherapy Surgery:No more than 35 days since prior definitive surgery Other:No other concurrent investigational agents [1] Susan Blaney, MD, Study Chair, Texas Children’s Cancer Center [2] Richard L. Heideman, MD, University of New Mexico Cancer Research and Treatment Center
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.