- What is Breast Cancer (Invasive/Infiltrating Ductal Carcinoma; IDC)?
- Statistics
- Risk Factors
- Progression
- Symptoms
- Clinical Examination
- How is it Diagnosed
- Prognosis
- Treatment
- References
What is Breast Cancer (Invasive/Infiltrating Ductal Carcinoma; IDC)?
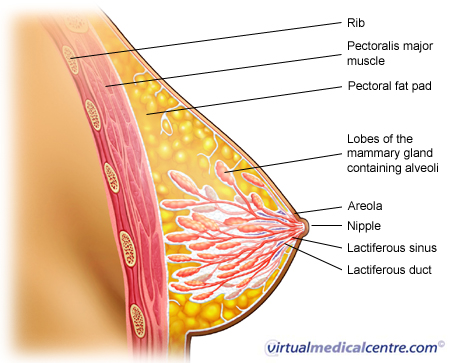
Ductal carcinoma of the breast is one of the main types of breast cancer. The breast is an organ designed to manufacture and deliver milk to the infant. The majority of the breast is composed of fatty tissue. Milk glands lie within this fatty tissue and are connected to the nipple via a series of ducts. The breast is also rich in blood vessels and lymphatic channels.
- Ductal carcinoma (70-80%): cancer cells that resemble the ducts of the breast
- Lobular carcinoma (5-10%): cancer cells that resemble the lobules or glands of the breast
- Medullary carcinoma (1 to 5%)
- Mucinous (1 to 6%)
- Tubular carcinoma (2%)
The types of breast cancer vary in their prognosis and the way in which they present.
Ductal carcinoma (invasive) will be discussed here.
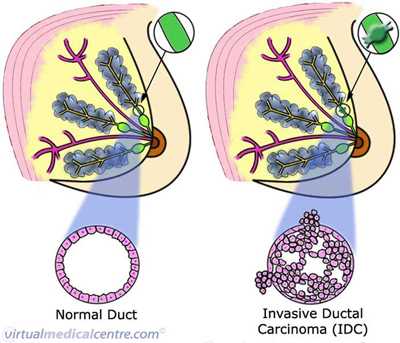
The images below show the cells of invasive breast cancer. These cells have not only multiplied out of control, filling the duct, but have also developed the ability to spread, or invade, beyond the lining of the ducts. This is invasive ductal carcinoma, or IDC.
 |
For information on ductal carcinoma in situ, see Pre-Invasive Ductal Carcinoma (DCIS). |
Statistics
Breast cancer is common. Breast cancer is one of the top two causes of cancer deaths together with lung cancer in most developed countries. Geographically, breast cancer is found worldwide.
99% of breast cancers occur in women with 1% in men.
Incidence increases with age. Breast cancer is rare in those under the age of 30, but presents in up to 1 in 14 women over the age of 70.
15-30% of breast cancers are of the in situ type whilst 70-85% are of the invasive type. Ductal carcinoma is the most common making up 80% of all breast cancers.
Risk Factors
The main risk factors for breast cancer are:
- Increasing age
- A family history of breast cancer
- Proliferative breast disease
- Hormonal factors: women who begin menstruation early, women who have a late menopause, late or few pregnancies, or who are obese. Some evidence is emerging that long term oestrogen therapy (for example, long-term use of the oral contraceptive pill, or hormone replacement therapy (HRT)) may increase risk, as may a diet which is high in fat.
- Others: exposure to radiation; geographical factors.
Progression
Invasive ductal carcinoma has developed the ability to spread beyond the ducts of the breast. Ductal carcinoma of the breast spreads initially by direct invasion of overlying skin and adjacent fat. Spread into lymphatics and to lymph nodes in the axilla is the most important step, since from there it can spread to lymph nodes in the neck and supraclavicular region and into blood vessels. Once in the blood vessels, spread is possible to distant organs such as the bones, lung or liver.
How is it Diagnosed
Any breast symptom, such as a lump or nipple discharge, is assessed with the ‘triple test’. This includes examination of the breast, imaging of the breast through mammography or ultrasound, and sampling of the breast tissue with fine needle aspiration (FNA), core biopsy or open biopsy.
Following a diagnosis of breast cancer, blood tests including Full Blood Count and Liver Function Tests may be used to assess the possibility that the cancer may have spread to the liver or bone marrow. Other imaging tests, including chest x-rays, bone scan, abdominal CT or liver ultrasound may also be used if symptoms suggest that the cancer has spread.
Prognosis
Early breast cancer has a good (greater than 80%) 5 year survival. Important prognostic factors which can help predict survival include involvement of lymph nodes, the size of the tumour, and how aggressive the tumour cells are.
If the cancer has metastasised (spread) to lung, liver or bone at diagnosis, 5-year survival rates are significantly lower.
Treatment
Surgical treatment of breast cancer aims to achieve total disease control through removal of the primary breast tumour, along with any local extension.
Surgical treatment can be divided into two major streams:
- Breast conserving surgery with complete local excision (CLE) and axillary dissection, or
- Total mastecomy with axillary dissection.
These two procedures are considered similar in terms of 5- and 10-year survival rates. The decision as to which procedure is more appropriate is therefore based on clinical features, such as the size and location of the tumour, and patient preference.
- Larger, widespread cancers or cancer near the nipple may usually require mastectomy (removal of the whole breast). This can be followed by reconstructive surgery.
- Smaller tumours, or tumours located in the outer quadrant in larger breasts may be removed by lumpectomy or partial mastectomy. Radiotherapy usually follows the procedure.
- Axillary dissection refers to the removal of lymph nodes in the axilla (armpit). These lymph nodes are commonly the first site of metastasis (spread) of a breast tumour, and axillary dissection is routinely done to ensure all cancer cells are removed. Rarely, with some very small and well-defined cancers, axillary dissection may not be necessary.
Adjuvant therapy refers to chemotherapy, radiotherapy or hormone therapy which is done with the aim of destroying any cancer cells not removed by surgery.
Chemotherapy protocols include:
- CMF:
- Cyclophosphamide 100mg/m2 PO days 1-14
- Methotrexate 40mg/m2 IV days 1+8
- 5-Fluorouracil 600mg/m2 IV days 1+8 (repeat every 4 weeks for 6 cycles)
ALL I.V. CMF:
- Cyclophosphamide 750mg/m2 IV day 1 (or 150mg/day)
- Methotrexate 60mg/m2 IV day 1
- 5-Fluorouracil 750mg/m2 IV day 1 (repeat every 3 weeks)
- AC:
- Doxorubicin 60 mg/m2
- Cyclophosphamide 600 mg/m2
- For High Risk Patients:
- TAC
- FEC 75
- FEC 100
- Docetaxel
- Paclitaxel
Modifications:
- Post menopausal:
- Tamoxifen 20 mg PO daily
- Locally Advanced FAC:
- 5-Fluorouracil 600 mg/m2 IV day 1 + 8
- Doxorubicin 60mg/m2 IV day 1 (vesicant)
- Cyclophosphamide 600mg/m2 IV day 1 (repeat every 4 weeks)
- Stage IV: First line chemotherapy:
- CMFP (oral or IV) (add prednisolone 40mg/m2 PO days 1-14 to CMF)
- Reassess every 3 courses Treat until maximum response
- Trastuzumab (Herceptin) and Taxanes
- Herceptin 4 mg/kg IV over 90 minutes then 2mg/kg/week over 30 minutes until progression
- WITH
- Docetaxel 75 mg/m2 IV over 1 hour every 3 weeks for 6 cycles OR
- Paclitaxel 90 mg/m2 IV over 60 minutes weekly
- CMFP (oral or IV) (add prednisolone 40mg/m2 PO days 1-14 to CMF)
- Herceptin single agent:
- Herceptin 4 mg/kg IV over 90 minutes then 2mg/kg/week over 30 minutes until progression
- Second line chemotherapy:
- Doxorubicin 60mg/m2 IV day 1 (vesicant) (repeat every 3 weeks)
- Third line chemotherapy:
- Docetaxel 75 mg/m2/day over 1 hour as starting dose can escalate to 100mg.m2/day IV over 1 hour. In heavily pretreated patients or those with poor liver function can start at 60 mg/m2. (repeat every 3 weeks)
- Docetaxel (weekly) 36 mg/m2/week over 1 hour for 6 weeks then 2 weeks off
- Paclitaxel 175mg/m2/day over 3 hours IV (repeat every 3 weeks)
- Paclitaxel (weekly) 100 mg/m2 IV over 1 hour
- Fourth line chemotherapy:
- Capecitabine 2500 mg/m2 divided into 2 doses daily po 2 weeks every 3 weeks
- Mitomycin C 10 mg/m2 IV Day 1 (vesicant)
- Vinblastine 5 mg/m2 IV Day 1 and 15 (vesicant) (repeat every 4 weeks)
- Hormonal Therapy:
- Tamoxifen 20 mg. po daily or Anastrozole 1mg po daily
- Then Medroxyprogesterone acetate 500 mg po daily Or Exemestane 25 mg/day
- Premenopausal Advanced Breast Cancer:
- Zoladex 3.6 mg SC every month
- Tamoxifen 20 mg/day
- Bone metastases: When the tumour has spread to bone, zoledronic acid can be used to help prevent fractures.
- Zoledronic acid 4mg iv over 15mins every 28 days
- Breast Cancer (Bone Predominant):
- Pamidronate 90mg IV over 2 hours.
If the tumour has spread to bone, treatment with zoledronic acid can help prevent tumour growth in bone and subsequent bone fractures. Symptoms that may require attention include bone pain from bone metastases, visceral (organ) pain from liver or lung metastases and neurogenic (nerve) pain if nerve tissue is compressed. Improvement in symptoms is an important measurement.
Hormone therapies:
Women with hormone receptor-positive tumours (eg. oestrogen-receptor positive tumours) should be offered adjuvant hormone therapies such as tamoxifen or ovarian ablation therapy.
More information
 |
For more information on breast cancer, types of breast cancer and its investigations and treatments, as well as some useful videos, see Breast Cancer. |
References
- Australian Institute of Health and Welfare & National Breast Cancer Centre 2006. Breast cancer in Australia: an overview, 2006. Cancer series no. 34. cat. no. CAN 29. Canberra: AIHW.
- Braunwald, Fauci, Kasper, Hauser, Longo, Jameson. Harrison’s Principles of Internal Medicine. 16th Edition. McGraw-Hill. 2001
- Cotran RS, Kumar V, Collins T. Robbins Pathological Basis of Disease Sixth Ed. WB Saunders Company 1999.
- Dr Guy Van Hazel, Oncologist, Mount Hospital, Perth
- Kumar P, Clark M. Clinical Medicine. Fourth Edition. WB Saunders, 1998.
- National Breast Cancer Centre. 2003. ‘The clinical management of ductal carcinoma in situ, lobular carcinoma in situ and atypical hyperplasia of the breast,’ First Edition. National Breast Cancer Centre, Camperdown,NSW. [online] Available from: http://www.nbcc.org.au/bestpractice/resources/CMW_dcisbook.pdf
- National Breast Cancer Centre. 2001. ‘Clinical practice guidelines for the management of early breast cancer:Second edition’. National Breast Cancer Centre, Camperdown,NSW. [online] Available from: http://www.nhmrc.gov.au/publications/synopses/cp74syn.htm
- Schwartz, GF, Solin, LJ, Olivotto, IA, et al. Consensus Conference on the Treatment of In Situ Ductal Carcinoma of the Breast, April 22-25, 1999. Cancer 2000; 88:946.
- Talley NJ, O’Connor Simon. Clinical Examination. Fourth Edition. MacLennan & Petty, 2001
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







