What is eosinophilic oesophagitis?
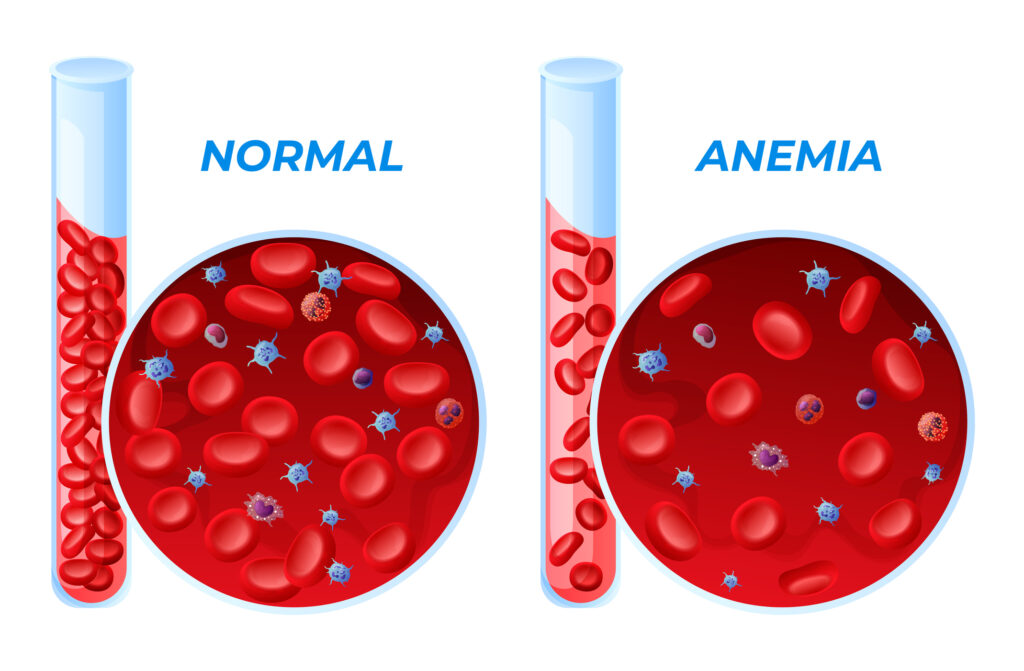
Eosinophilic oesophagitis (EE) is an allergic condition in which elevated levels of eosinophils (white blood cells that are part of the immune system) in the oesophagus cause inflammation. This in turn leads to damage of the oesophageal tissues. People living with the condition have difficulty swallowing and often experience food bolus impaction, that is food getting stuck in their throat.
Although EE is a major cause of gastrointestinal illness, it has only been recognised as a distinct condition in recent decades. Previously it was diagnosed as gastro-oesophageal reflux disease, a non-allergic condition characterised by the reflux of stomach acid into the oesophagus. As a result, research about the management and treatment of the condition is still in the early stages.
Food stuck in the throat
Tim was recently diagnosed with EE after an episode in which he was hospitalised when food got stuck in his throat. He shared his experience finding out he had the condition and developing a strategy for managing the symptoms.
“I was diagnosed with EE almost a year ago, in my thirties,” Tim said. “I was taken to hospital by ambulance when a lump of rice got stuck in my throat. It was frightening. I could still breathe but the food in my throat made breathing difficult.”
Food allergy and food restriction
Like many people who are diagnosed with EE, Tim had a history of allergic disease. “I’d experienced food allergies and difficulty swallowing all my life,” he said. “I almost went into anaphylactic shock as a baby after eating peanut butter and was only able to eat pureed food until I was four years old. So it wasn’t completely unusual for me to have trouble getting food down.”
“I had been on a restricted diet, avoiding foods I was allergic to for more than ten years when this happened, eating plain boiled rice. I have food allergies and food intolerances to foods containing nuts, gluten and other various food and environmental triggers. Some days, by the afternoon, the EOE was so painful that I couldn’t eat or swallow.”
However Tim’s symptoms seemed to be worsening. He had experienced food impaction several times in the twelve months before the hospital admission that eventually led to his EE diagnosis.
“There were other occasions the food lump eventually passed through to my stomach. This time I could feel the lump of rice in my throat and it wouldn’t move. It was really painful, like the worst indigestion you can imagine. The acid build up was burning in my oesophagus. I was also getting chest pains.
“When I arrived in hospital I had to drink water to try and push the rice out. When that didn’t work I was given a fizzy drink and had to drink it all quickly. This induced vomiting and dislodged the rice.
“Because I had the chest pains they also did an ECG at the hospital to check for heart problems. It showed my heart was okay but didn’t explain why I kept getting food stuck in my throat.”
Get on top of your general health
Find and instantly book affordable GPs within Australia
Getting diagnosed with eosinophilic oesophagitis
After being discharged from hospital, Tim went to see a general practitioner to further investigate what was causing the continual, and quite frightening, experience of food getting stuck in his throat.
“The doctor referred me to a gastroenterologist for further tests. The specialist did an endoscopy and a biopsy of my oesophagus. The pictures taken in the endoscopy showed that my oesophagus was narrowing and from the biopsy we found out that there were high levels of eosinophils in my oesophagus. I was diagnosed with eosinophilic oesophagitis.
“I was relieved to be diagnosed – at least I knew what was causing the problems. The cost of the endoscope and biopsy was around $450. And it was really just the beginning – I had the diagnosis but this was the start of eliminating trigger foods from my diet and to manage the symptoms through different drug therapies.”
Starting treatment
“When I was diagnosed the doctor prescribed a medication called Pariet to reduce the amount of acid in my stomach. At first it really reduced the symptoms and I was able to eat more. I even joined the gym and gained 5kg of muscle working with a personal trainer.
“Unfortunately it didn’t last for long. The medicine just seemed to stop working, about six months after I started taking it and my old symptoms returned. Twice in a single month we had to call the ambulance to the farm when food got stuck in my throat. The first time my throat was so tight and inflamed, beef mince I was having for dinner was lodged in my throat. Then a few weeks later, I had an allergic reaction to milk that I had on some gluten free weet-bix made from sorghum, as I suspected milk to be one of the trigger foods, causing this problem.”
Identifying trigger foods
The next option for Tim was working with allergy specialists and dieticians at the RPAH allergy unit, to try and establish which foods were triggering his allergic symptoms. “They started by giving me a different medication, a puffer similar to the ones people with asthma use called Flixotide. It’s reduces inflammation in my oesophagus. But they also suggested we do further tests to identify trigger foods.
“There are a couple of ways they test for food allergies, one is by doing skin prick tests to see if there is an allergic reaction to true allergies and the other is by eliminating foods that seem to be triggering the symptoms and seeing if these symptoms reduced and hopefully lower my eosophil count.
“I was in a difficult position because my diet was already restricted, but skin prick tests are not always accurate. For example I’d had plenty of allergy skin prick tests in my life, and apart from one in 2003, they all indicated I wasn’t allergic to cow’s milk and rice. So I drank rice milk, ate plain rice and plain yoghurt on a daily basis. However rice kept getting stuck in my throat. Even though it’s not an allergic trigger for most people, rice seemed to be triggering my symptoms so I cut that out of my diet, even though the skin prick tests were negative.
“Eggs and dairy products pretty common trigger foods for people with Eosinophilic oesophagitis. First I eliminated dairy, even though yoghurt was a big part of my diet – I used to eat a kilo of low fat yoghurt for breakfast and it was a major part of my calorie intake. My symptoms improved but I could still here a strange gurgling noise in my throat when I swallowed, something like the gurgling noise water makes when it’s going down a sink that’s blocked.
“The next foods to go were eggs and rice and thankfully the gurgling noise also went away when I stopped eating them. But it was becoming more difficult to eat enough. My diet was restricted to lean meat, pears and a few vegetables like potatoes, choko and Brussel sprouts.”
Maintaining energy intake with food replacement supplements
Under the guidance of the dieticians at the RPAH Allergy unit, Tim added an elemental formula to his diet. “It’s a high-energy powder with all the vitamins and calories that most people get from food. The one I use is called Nutricia Elemental 028 extra unflavoured. You can get flavoured powders, but sometimes the flavours trigger allergies so the dietician recommended that I use the unflavoured version.
“I mix it with water and drink it like a protein shake, using three sachets a day to keep my energy intake up.
“The down side of the elemental diet is the cost. The powder comes from the UK and I can only get it posted from their Sydney office. It’s not covered by the Pharmaceutical Benefits Scheme (PBS), so I have to pay the full cost. Each box of Elemental 028 extra has 10 sachets which costs $135.50. I order 3 boxes that would last around 10 days costing $406. That’s quite difficult to afford, when I’m on a low income.”
Lifestyle changes
“I moved back to my parent’s farm about ten years ago when my symptoms were out of control. I didn’t want to live alone. I needed the support. I see my friends getting careers and getting married, but it’s like my life is stuck in limbo. I’m in the process of eliminating trigger foods in managing EE.
“The symptoms I get from EE have made it difficult to study or work, because I can’t always eat as much as I should be eating, and my carbohydrate intake is restricted, my energy levels are often low. Doing physical work like lifting is difficult.
“Living with EE also affects my social life. The last time I went to a restaurant was about four years ago. I couldn’t eat anything on the menu so I just had to sit there. It’s difficult, sitting there watching everyone else eat.
“I haven’t been in a relationship for years as a result of the challenges that many people in society would not relate too. Managing my symptoms and food getting stuck in the oesophagus on a regular basis, has been a difficult adjustment. You lose confidence and sometimes feel really isolated. I don’t have much of a social life anymore, which makes it difficult to meet new people.”
Getting involved in eosinophilic oesophagitis advocacy
However now that Tim has a diagnosis, and can put a name to the condition that causes his symptoms, he’s keen to get involved in raising awareness about EE.
“It’s a condition people don’t know much about. I’d never heard of EE until I was diagnosed. Now I’ve gotten in touch with AusEE, an organisation that raises awareness and funds towards research of Eosinophilic disorders and supports people who have the condition. I’m planning to get involved in a support group so I can meet other people who have had the same experiences.
“I also want to get involved in raising awareness about the condition, so that more research is done to find a cure while adults with EE get better support. Therefore I’m interested in raising awareness about the elemental formulas adults need as part of their treatment, and the lack of support in comparison to children with EE. It’s a necessity and I need them to survive, but Elemental 028 is not on the PBS. Maybe by raising awareness, adults would get some support from the government as a result.
“There is research being conducted about EE and food allergies, to discover better ways of diagnosing and treating them. I’m interested in being involved in research and being a part of finding a cure, or at least better ways of managing EE and other related allergic conditions. I have EE but I’m not going to just sit back and live with it. I want to share my experience and be involved in making it easier for people with EE to live a better life.”
Advice to other people living with EE or experiencing symptoms
“Getting my diagnosis hasn’t made the problem go away, but I feel better knowing the condition causing my symptoms. For other people who have difficulty swallowing or have a food bolus episode, I’d recommend that they see their doctor and request a referral to have further tests done with a gastroenterologist and allergist to further investigate problem foods or environmental triggers they may be a problem. They may recommend drug therapy in conjunction with eliminating and avoiding allergy triggers as this is the best course of treatment at the moment. Keep a food and symptom’s diary and talk to your allergist and dietician if you have suspicions around certain foods.
“If you’re diagnosed with EE, get in touch with a support organisation like AusEE. It’s not only a way of finding other people going through the same thing. It’s also a way of raising awareness about the condition.”
More information
 |
For more information on how the body and immune system responses to allergies, see Allergy and the Immune System. |
 |
For more information on risk factors, symptoms and treatment of food allergy, see Food Allergy. |
 |
For more information on what is involved in an endoscopy procedure and how to prepare for one, see Upper Gastrointestinal Endoscopy. |
References
- Mayo Clinic. Eosinophilic oesophagitis. 2014. [cited 23/08/2015]. Available from: [URL Link]
- American Academy of Allergy, Asthma and Immunology. Eosinophilic Oesophagitis. 2015. [cited 26 August 2015]. Available from: [URL Link]
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.