Risk Assessment
There are several risk assessment charts available to assess a patients’ risk of developing a pressure ulcer. These include: the Norton Scale, the Braden Scale and the Gosnell Scale. Many hospitals have modified these scales to suit their settings. The scales allow the caregivers to assess the individuals risk and allow preventative measures to commence on admission. It is important to assess an individuals risk and complete a written care path to suit. Documentation of preventative measures and regular records should be made throughout and regular re-assessments should be conducted.
Skin Care
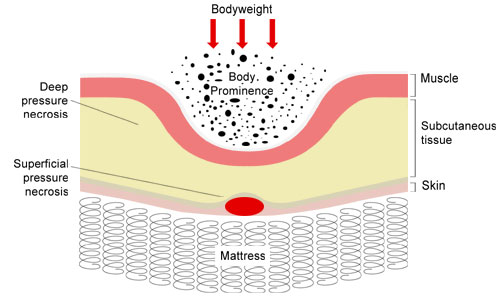
The maintenance of skin integrity is the best way to minimise the risk of skin breakdown. Healthy skin should be clean, dry and well hydrated. Good skin care practices should include:
- Daily inspections of the skin, paying particular attention to bony prominences.
- Observation and palpation techniques should be used to inspect areas for changes in: colour, firmness, skin temperature, sensation.
- Maintain skin hygiene through regular gentle cleansing and thorough drying. Avoid irritating soaps or cleansing agents.
- Use moisturises on dry skin.
- Don’t massage bony prominences as this may lead to tissue damage as a result of friction.
- Use protection and padding such as sheepskin booties and elbow pads. Care should be taken in the selection of padding, avoid using donut shaped devices.
- Protect the skin from maceration. Remove the source of moisture. For example; excessive sweat, wound drainage, urine and faeces.
- Plastic sheeting and incontinence pads should be avoided wherever possible or changed at the earliest possible opportunity.
- It may be appropriate to seek a medical review for the incontinent patient to control or limit the amount of incontinence.
- Minimise skin injury resulting from friction, through the use of protective dressing and lubricants.
- Educate the patient regarding skin care and the importance of repositioning.
- Use protective devices to keep bony prominences from direct contact with each other. For example pillows between the knees.
- Ensure linen is not bunched up under the patient and that dressings are not folded or scrunched.
- Use pressure relieving/ reducing devices such as air mattresses (static air, alternating air, gel, water mattresses) in high risk patients.
Other Considerations
Moving and Handling:
- Improved manual handling techniques and appropriate training is important to minimise the risk of pressure ulcers.
- Use proper transferring and turning techniques. Use devices such as slide sheets and hoists to minimise skin trauma.
- Regular repositioning of patients every 2 hours when bed bound (if there are no contraindications) and every hour or more when positioned in a chair. Educate the chair bound patient to reposition or weight shift every 15 minutes.
- When appropriate, provide the patient with an overhead trapeze or side railing.This may aid their ability to reposition themselves independently.
- Keep the head of the bed at the lowest possible height, not raised more than 30 degrees (unless contraindicated).
- When positioning the patient in the lateral position, do not place them directly on their trochanter.
Nutrition:
- Adequate nutrition is important in preventing and promoting wound healing.
- Assess the patient’s nutritional status during admission.
- Encourage adequate intake.
- Educate the patient regarding nutrition and hydration.
- Documentation may be required to accurately assess intake. Maintenance of fluid balance and intake charts will assist this process, also daily weighting may be appropriate.
- Seek a medical review or dietician assessment to evaluate the patients’ nutritional status.
- Nutritional deficiencies may need correcting. Supplements may be required, particularly protein intake, calorie intake as well as vitamin A, C, E.
Other Important Considerations:
- Keep the patient as active as possible. Encourage ambulation and regular exercises etc.
References
Kindly Supplied by Virtual Nursing Education.
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.