- What is Cardiac Tamponade
- Statistics on Cardiac Tamponade
- Risk Factors for Cardiac Tamponade
- Progression of Cardiac Tamponade
- Symptoms of Cardiac Tamponade
- Clinical Examination of Cardiac Tamponade
- How is Cardiac Tamponade Diagnosed?
- Prognosis of Cardiac Tamponade
- How is Cardiac Tamponade Treated?
- Cardiac Tamponade References
What is Cardiac Tamponade
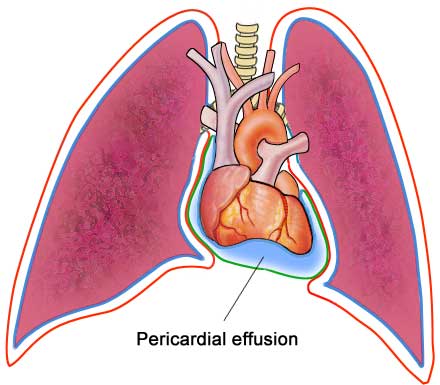
Cardiac tamponade is the compression of the heart caused by blood or fluid accumulating in the space between the myocardium (heart muscle) and the pericardium (the outer covering sac of the heart). This is a medical emergency, with increasing fluid producing elevated pressures on the heart and preventing proper filling. If left untreated, the heart’s pumping chambers (ventricles) are compromised, resulting in shock and death.
How does cardiac tamponade result?
The pericardium is a thin double layered sac which encloses the heart. The inner layer is called the visceral pericardium. This is thin and watery in constitution. The outer layer is called the parietal layer – a tougher layer attached to other body organs like the diaphragm and cartilages between the ribs.
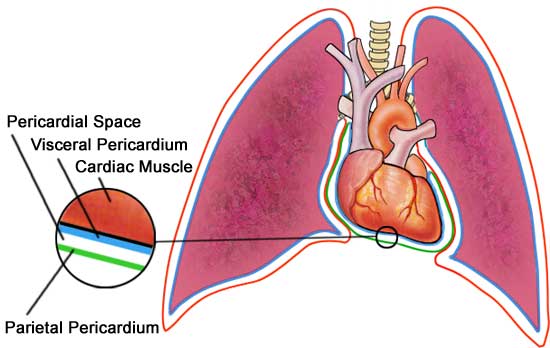
Fluid is contained within the layers (in an area called the pericardial space) and lubricates the two surfaces which constantly rub together. There is about 20ml of fluid in this pericardial space. When fluid builds up slowly, more than 2000mls can be accompanied in the space, before any changes are noticed.
If the fluid builds up quickly, as little as 200mls can trigger decompensation of the heart. Increased fluid results in increased pressure, which can decrease the efficiency of the heart’s pumping mechanisms and lower the body’s blood pressure.
Statistics on Cardiac Tamponade
Cardiac tamponade occurs in approximately 2 out of 10,000 people. The reported incidence of acute pericardial tamponade is approximately 2% of penetrating trauma.
Risk Factors for Cardiac Tamponade
There are many reasons why you might have a cardiac tamponade.The three most common causes of cardiac tamponade are malignancy, uraemia (a toxic condition resulting from kidney disease due to retention in the bloodstream of waste products normally excreted in the urine), and irritation of the sac surrounding the heart, due to unknown causes.
Malignancy:
If you have cancer, fluid can accumulate in the pericardial sac surrounding the heart. This fluid can build up and cause an increased pressure on the heart. Cancers can also cause bleeding into the pericardial sac. This build up of blood in a confined space can further compromise the heart.
Penetrating or Blunt Injury:
A penetrating cardiac injury such as a stab wound to the chest, can result in leakage of blood into the pericardial sac (known as haemopericardium) and cause a rapid rise in the pressure around the heart.
Iatrogenic causes:
Occasionally, cardiac tamponade can be a result of medical interventions and procedures. These include; during central line placement, cardiac catheterization and pacemaker insertion.
Heart Attacks (Myocardial infarction):
After a heart attack, your heart muscle is weaker and more likely to rupture around the site of tissue that has sustained injury.
Infection:
Cardiac tamponade is often associated with pericarditis (inflammation of the pericardial sac) caused by bacterial or viral infections.
Progression of Cardiac Tamponade
Tamponade is a life threatening condition if untreated. The outcome is often good if the condition is treated promptly and the underlying cause is resolved. However, tamponade may recur.
Symptoms of Cardiac Tamponade
If you are affected by cardiac tamponade, some of the following symptoms may be experienced;
- anxiety,
- shortness of breath,
- fatigue,
- chest discomfort, and/or chest pain. The pain may be; sharp, stabbing, radiating into the neck, back or abdomen. Often it is worsened by deep breathing or coughing or laughing.
- Palpitations (awareness of the heart beating faster, stronger or at a different pattern compared to usual)
- feeling faint, light-headed.
In traumatic cardiac tamponade, there may be history of an obvious penetrating chest injury. In these circumstances, you may be acutely short of breath and may become confused and drifting in and out of consciousness.
If you are affected by cardiac tamponade, you may also have a history of medical diseases that can involve the sac surrounding the heart, such as end-stage kidney disease.
Clinical Examination of Cardiac Tamponade
When the doctor examines you, he or she may find the following signs. In severe, acute situations, such as heart trauma or rupture, there is a decrease in the pressure in your arteries, an increase in the pressures of the veins and soft heart sounds. Signs of cardiac tamponade are influenced by the volume and rate of accumulation of fluid.
In circumstances where the rate of accumulation of fluid is slow, you may have some signs such as; shortness of breath (especially when lying down), liver enlargement and an increase in pressure in the jugular vein (one of the main veins running down the side of the neck). These signs are similar to those found in patients with heart failure.
The clinical triad of low blood pressure, increase in pressure in the jugular vein and soft heart sounds is known as Beck’s triad. This is very suggestive of cardiac tamponade.
How is Cardiac Tamponade Diagnosed?
These tests may be helpful in helping determine the presence and cause of cardiac tamponade.
Lab Studies:
- Full blood picture – blood is taken to measure the level of haemoglobin, red cells, white cells, etc.
- Creatine kinase and isoenzymes – Enzymes released when heart muscle is damaged, such as CK-MB, Troponin T/I, may be elevated.
- ECG – provides an electrical picture of the heart and can demonstrate low voltages and/or alternating sizes of complexes.
Imaging Studies:
- Chest x-ray: The heart may appear large, globular or pear shaped with sharp outlines. In cardiac tamponade, the chest x-ray may demonstrate an enlarged heart shape after 200-250 mL of slow fluid accumulation. A normal cardiac picture seen in patients with rapid accumulation of fluid or blood.
- Echocardiography: Most useful technique for demonstrating fluid in the pericardial sac and can show collapse of the right pumping chamber of the heart (ventricle) when the heart relaxes.
- Doppler: May show increased flow through specific valves in the heart.
- Magnetic Resonance Imaging: May detect blood or fluid around the heart.
Prognosis of Cardiac Tamponade
The prognosis for patients with cardiac tamponade depends upon the cause of the tamponade. For penetrating injuries, the outcome depends heavily upon the quickly diagnosing and treating tamponade. Factors that indicate a better prognosis include; minor injuries, isolated injuries only to the right ventricle and blood pressure values that are aren’t too low.
How is Cardiac Tamponade Treated?
Treatment of a cardiac tamponade depends on the haemodynamic stability of the patient and the status of the underlying malignancy.
The mainstay of treatment is drainage of the pericardial fluid (pericardiocentesis), preferably under echocardiographic guidance, to relieve the pressure. Drainage of as little as 30-50ml of fluid may result in a dramatic improvement in symptoms. If untreated, cardiac tamponade may lead to pulmonary fluid collections, shock and even death. However, with prompt recognition and treatment, most patients recover well. Patients require close monitoring, usually in an intensive care unit.
As for all patients with chest pain, oxygen and ECG monitoring should be applied. Adequate blood volume should be maintained with blood, plasma or other fluid products. Elevating the legs may also assist venous return, which is decreased due to compression of the heart. Drugs affecting heart contractility (inotropic drugs) may be used to increase cardiac output without increasing resistance in the peripheral blood vessels.
Recurrent tamponade may require treatment with surgery. This may involve the creation of a communication between the pericardial and pleural spaces, or creation of a shunt between the pericardial space and the abdominal cavity (pericardio-peritoneal shunt). An alternative is pericardiodesis, where an intrapericardial catheter may be used to introduce drugs that will cause the two pericardial layers to fuse together. Very occasionally complete removal of the pericardium (pericardiectomy) may be required. Invasive surgery may not be used if the patient’s underlying cancer is likely to result in death in a short time.
Cardiac tamponade is rarely the initial presentation of malignancy, and investigation including analysis of pericardial fluid usually reveals the cause. Full blood count, blood film, serum chemistry, and cancer markers may assist diagnosis. Pericardial effusion from malignancy mostly contains blood or blood and serous fluid. The fluid must be examined for malignant cells, and false negative results are uncommon, but may occur in patients with lymphoma or mesothelioma. The presence of lymph fluid may indicate a mediastinal lymphangioma.
Cardiac Tamponade References
- Kasper DL. Harrisons Principles of Internal Medicine. New York: The McGraw-Hill Companies; 2006
- Kato N. Cardiac Tamponade [online]. 2006 [cited 2006 April 25th]. Available from: URL: http://www.nlm.nih.gov/medlineplus/ency/article/000194.htm
- Longmore JM, Hope RA, Longmore M. et al. Oxford Handbook of Specialties; USA: Oxford University Press Inc. 2001
- Valley VT, Fly CA. Pericarditis and Cardiac Tamponade. E-medicine [serial online]. 2005 [cited 23rd April 2006]. Available from URL: http://www.emedicine.com/EMERG/topic412.htm
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







